Speech Treatments and Services
Inpatient
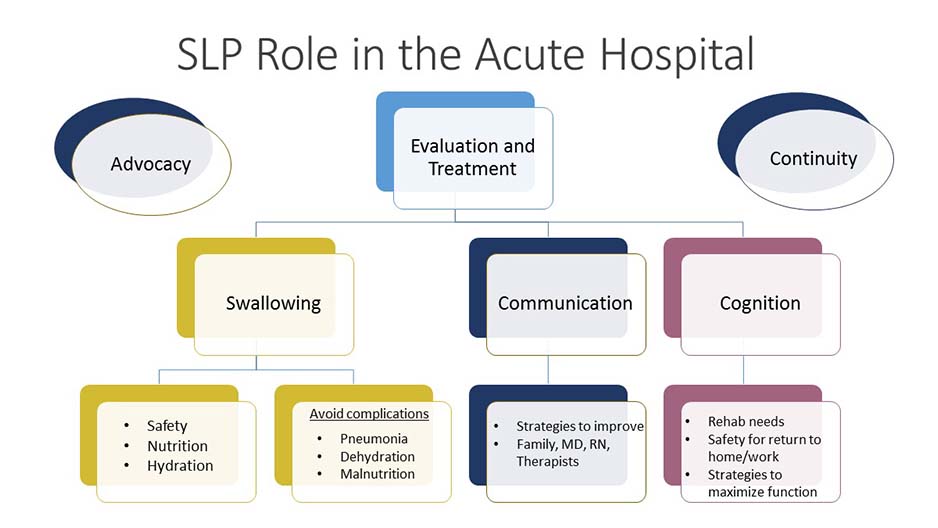
Our Role
In the hospital setting speech-language pathologists (SLPs) play a unique role as part of the interdisciplinary care team. We specialize in assessing and managing the speech, language, communication, cognition, feeding and swallowing related difficulties of adult and pediatric patients affected by injury or illness. Swallowing evaluation includes a comprehensive clinical assessment at the bedside, as well as Videofluoroscopic Swallowing Study (VSS) or a Fiberoptic Endoscopic Evaluation of Swallowing (FEES). You can learn more about these procedures below in the "Instrumental Evaluation" section.
Our inpatient staff are available seven days a week.
Our Values
- Individualized care based on patients’ needs and the changing complexities of the illness, whether in the intensive care unit (ICU) or a medical, neurology or surgical step-down unit
- Collaborative decision making
- Strong interprofessional relationships
- Excellent communication with those caring for our patients at the bedside
- Patient advocacy
Our Presence
Medical teams across the entire hospital may consult the inpatient team for a variety of conditions including:
- Stroke, brain injury, brain tumor and aneurysm
- Neurodegenerative disorders including ALS, Parkinson’s Disease and dementia
- Oncology
- Artificial airways (tracheostomies and/or ventilator-dependent); airway reconstruction
- Complex medical conditions such as respiratory difficulties, cardiac disease, esophageal disorders, transplant and burns
- Premature infants and neonates
- Adult and Pediatric trauma
Our Professional Development
Inpatient team members are involved in training the next generation of SLP’s, collaborating with the MGH Institute of Health Professions, and actively pursuing professional development and lifelong learning in myriad ways including:
- Weekly swallowing rounds
- Boston area quarterly Dysphagia Grand Rounds
- Participating in Interdisciplinary Rounds on Neurology, Surgery, Intensive Care and Medicine units throughout the hospital
- Membership on hospital-wide committees, including Optimum Care Committee, Comprehensive Stroke Quality Team (CSQT) and multiple Collaborative Governance committeesCognition
Outpatient
The Mass General Department of Speech, Language and Swallowing Disorders & Reading Disabilities ensures comprehensive specialized outpatient services that are provided at three sites: Main Campus, MGH Chelsea HealthCare Center and MGH Revere HealthCare Center.
Adult Swallowing Service
Housed in our main campus site, the outpatient swallowing service provides expert diagnostic and treatment services to adults with swallowing disorders. Difficulty swallowing may arise from a variety of causes including:
- Cancer of the head and neck
- Neurologic conditions such as stroke and brain tumor
- Degenerative neurologic disease such as Parkinson’s disease, motor neuron disorders like ALS, and Huntington’s disease
- Respiratory problems such as COPD
Swallowing function is typically evaluated by completing a fluoroscopic Video Swallowing Study (VSS). During this study the speech-language pathologist collaborates with radiology staff to take images as the patient swallows various consistencies of barium.
Fiberoptic Endoscopic Evaluation of Swallowing (FEES) may be also performed to evaluate the function of the voice box and throat during swallowing.
Individualized treatment is based on the specific findings of the evaluation and is tailored to each patient’s need in collaboration with the patient, family and healthcare provider. Our treatment is driven by best clinical practices and is evidence-based. We focus on improving the safety of oral intake, making eating easier and more efficient, reducing the risk for aspiration and maintaining quality of life. Treatment may include strengthening exercises, diet modification, biofeedback (sEMG) and respiratory muscle strengthening to improve airway protection.
Our swallowing specialists are actively involved as members of multidisciplinary care teams, including:
- Multidisciplinary Head and Neck Oncology Team
- Huntington’s Disease and Movement Disorders Unit
- ALS Multidisciplinary Clinic
Adult Speech, Language and Cognition Service
Comprehensive services are provided at our main campus site for adults who have suffered a neurologic injury from a traumatic event or an acquired brain injury including stroke, brain tumor and aneurysm. We also treat patients with neurodegenerative disorders such as ALS and Multiple Sclerosis and movement disorders including Parkinson’s and Huntington’s disease.
Our highly specialized staff are skilled at assessing and treating patients experiencing cognitive and speech-language disorders that include:
- Attention, memory, problem solving and executive dysfunction
- Aphasia and Primary Progressive Aphasia
- Motor speech disorders
- Voice disorders caused by Parkinson’s disease including:
- Lee Silverman Voice Treatment (LSVT).
- SPEAK OUT! and LOUD Crowd, as developed by the Parkinson Voice Project
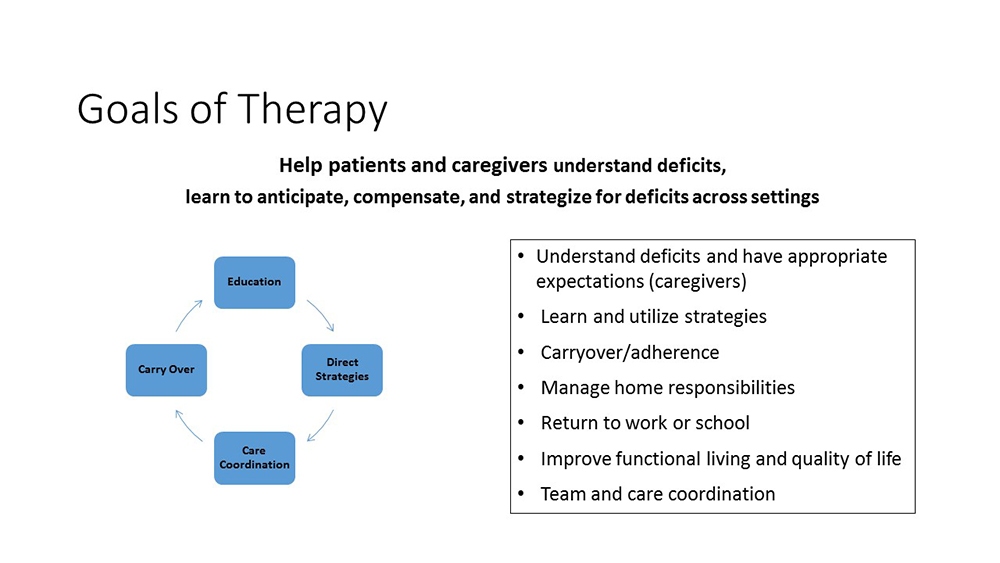
Treatment is focused on increasing functioning at home and in the community, supporting successful return to work and improving quality of life.
Our SLP’s are actively involved as members of multidisciplinary care teams, including:
Pediatric Feeding and Swallowing Service
We provide comprehensive services for infants, toddlers, children and adolescents with feeding and/or swallowing disorders (dysphagia) at our main campus site, and feeding treatment in the health centers. Feeding issues may be the result of reduced oral motor skills, differences in oral sensitivity, difficulty tolerating a variety of textures, slow progression to solid foods or feeding problems that delay development or feeding milestones. The presence of respiratory, neurological or cardiac problems can disrupt swallow coordination. Feeding evaluations are conducted by a speech-language pathologist or by a multidisciplinary team, depending on the nature of the feeding concern. The team includes clinicians from the disciplines of gastroenterology, occupational therapy, psychology and nutrition.
Diagnostic evaluations may involve imaging of swallowing function with a fluoroscopic Video Swallowing Study (VSS) . During this study a speech-language pathologist collaborates with pediatric radiology staff to take images as the child swallows various consistencies of barium to assess swallow function. Learn more.
Our speech-language pathologists also evaluate children as part of the following interdisciplinary clinics and services at MassGeneral Hospital for Children:
- Cleft Lip and Craniofacial Clinic
- Newborn Developmental Follow-Up Clinic
- Pediatric Airway, Voice, and Swallowing Clinic
Pediatric Speech and Language Service
Our pediatric speech-language pathologists evaluate and treat children with communication delays and disorders in our outpatient main campus setting (birth to age 6), and at community health centers in Chelsea and Revere (birth to age 18). Areas addressed include:
- Speech sound production (articulation, phonology, Childhood Apraxia of Speech)
- Expressive and receptive language (talking and understanding)
- Written language (reading, writing)
- Fluency (stuttering)
- Executive functioning
- Social interaction/pragmatics (including autism spectrum disorders)
- Velopharyngeal insufficiency/nasality (VPI)
Bilingual speech-language pathologists serve Spanish, Portuguese, and Russian speaking children in the MGH Chelsea and Revere Health Care Centers. English speaking speech-language pathologists work with medical interpreters to serve speakers of other languages at all three centers. When concerns about communication and academics arise, a child may be referred for a comprehensive evaluation to establish the child’s communicative profile, make appropriate recommendations and referrals, and determine next steps. We also work in conjunction with outside agencies such as Early Intervention and local school districts to provide family-centered, comprehensive care.
Speech and language therapy services at MGH are intended for short-term intervention, followed by a transition plan for children from outpatient hospital services to school systems and/or communities.
Our clinicians are active members of a variety of multidisciplinary teams including the following clinics:
- Developmental NeuroPediatric Clinic
- Down Syndrome Clinic
- Newborn Developmental Follow-Up Clinic
- Pediatric Therapy Team
Specialty Clinics
Our speech-language pathologists work closely with your physician and other healthcare team members to provide an integrated approach to care. We can provide co-treatment sessions with other disciplines and work with your team of specialists in the following clinics:
Airway, Voice and Swallowing Center
This multidisciplinary center comprises clinicians from speech language pathology, otolaryngology, gastroenterology and pulmonary disciplines. This highly specialized team manages airway, swallowing and voice disorders in the pediatric population. The SLP provides brief feeding or speech/ voice assessment during the clinic visit. Depending on the needs of the patient, a Videofluoroscopic Swallowing Study may also be performed the same day. Recommendations are provided for management and care of identified airway, voice or swallowing issues. Learn more.
ALS and Huntington’s Disease Clinics
Designated clinicians with an expertise in the care of patients whose speech, language and/or swallowing may be affected as a result of a neurological disease participate in routine multidisciplinary clinics that care for patients diagnosed with ALS and with Huntington’s Disease. SLPs actively participate in assessment, intervention, patient/family education and support and clinical research. Learn more.
The Center for Nutrition and Feeding
SLPs work as members of an interdisciplinary team that provides assessment of pediatric feeding and swallowing problems. Typical referrals include children with failure to thrive, medically complex issues that impact feeding performance, and GI issues such as reflux, delayed gastric emptying, esophageal dysmotility, and food allergies/ sensitivities. The team evaluation includes a medical and feeding history intake and observations of the child during feeding activities. If there are concerns with swallowing safety, Videofluoroscopic Swallowing Study can be arranged. Learn more.
Cleft Palate/Craniofacial Team
This multidisciplinary group provides evaluation services to patients with craniofacial and cleft lip or palate anomalies. In addition to speech-language pathology, the team includes clinicians from pediatric surgery, genetics, dentistry, oral maxillofacial surgery, plastic surgery and otolaryngology. Additional assessments through the Speech, Language and Swallowing Disorders Department may be scheduled for more in-depth needs. Learn more.
Developmental Neuro-Pediatrics (DNP)
The Developmental Neuro-Pediatrics DNP Program provides comprehensive assessments of children between 18 months and 6 years of age suspected of having developmental delays, autism spectrum disorder and complex neurodevelopmental conditions, including genetic disorders. The SLP performs a comprehensive speech-language evaluation and works closely with the team to guide treatment recommendations. The multi-disciplinary team comprises a pediatric neurologist, pediatric neuropsychologist, speech and language pathologist, occupational therapist and physical therapist. Learn more.
Down Syndrome Clinic
The Down Syndrome Program provides compassionate and comprehensive care through a multi-disciplinary approach. The Down Syndrome Program has five distinct clinical services which provide specialty care that is specific to the patients’ age group, from prenatal services through adulthood. Families will be educated about Down syndrome and comprehensive supports will be provided for their child’s needs as well as supported about transition planning to adulthood. Learn more.
Head and Neck Cancer Clinic and Tumor Board
The SLP is an integral member of the interprofessional Head and Neck Cancer team which includes ENT surgeons from Massachusetts Eye and Ear and medical and radiation oncologists and their nurses from Mass General. Patients with newly diagnosed cancer of the head and neck attend one of two weekly clinics during which SLPs evaluate and counsel patients who have current swallowing or speech difficulties, as well as those whose communication and/or swallowing may be affected by the planned treatment. During Tumor Board meetings where treatment plans are discussed the SLP provides knowledge and expertise on the likely impact of the tumor or the proposed treatment on swallowing and speech function. Learn more.
Newborn Developmental Follow-Up Clinic
The Newborn Developmental Follow-Up Clinic provides services to at-risk infants from birth to two years who may be at-risk if born earlier than the due date (premature) or with serious unexpected medical problems. Experts in taking care of at-risk infants include a neonatologist, pediatric nurse practitioner, occupational therapist and speech-language pathologist. The Newborn clinic works closely with primary care doctors to provide comprehensive care addressing growth and development, nutrition, medical, neurological and developmental problems. Learn more.
Pediatric Therapy Team (PTT)
Pediatric patients who have weaknesses in communication, gross motor, sensory and fine motor skills may benefit from a PTT evaluation. We see children with a variety of diagnoses, such as ADD, ADHD, cerebral palsy, developmental delay, dyslexia, learning disabilities, Pervasive Developmental Disorder/Autism Spectrum Disorder, Seizure Disorder, and Sensory Integration Impairments.
The PTT evaluation is a multidisciplinary, same-day assessment completed by a Speech-language Pathologist, an Occupational Therapist, and a Physical Therapist. This provides ease of scheduling, convenience of a single day appointment, coordinated evaluations and integrated recommendations in a single, comprehensive report.
Disorders
Comprehensive services include evaluation, treatment, intervention, prevention and consultation.
- Oral-pharyngeal swallowing
- Pediatric feeding and swallowing
- Speech (articulation, fluency/stuttering, voice, dysarthria and resonance)
- Speech sound production (articulation, apraxia)
- Cognitive aspects of communication including attention, memory, problem-solving and executive functions
- Acquired language disorders (Aphasia)
- Expressive (talking) and receptive (understanding) language delays
- Social/pragmatics (including Autism Spectrum disorders)
- Language-based learning disabilities (reading, spelling, and writing)
- Velopharyngeal insufficiency, nasality and resonance
- Fluency/stuttering
Instrumental Evaluation
An instrumental swallow evaluation gives us more information and helps to understand the extent and the nature of the problem. This allows for an individualized treatment plan to be determined by the therapist in collaboration with the patient and family. We offer several instrumental evaluations as below.
Video Swallowing Study (VFSS)
A video swallowing study takes place in the radiology department along with the SLP and radiology staff. Some additional names used for this test are:
- Videofluoroscopic swallowing study or videofluoroscopy
- Modified barium swallow or MBS
- Cine-esophagram
What is a VFSS?
- Uses a video x-ray to see what happens during swallowing
- Looks at the mouth, throat and parts of the esophagus during sucking (infants), chewing, drinking and swallowing
- Looks at the safety of swallowing different types of food and liquid
- Helps determine the reason (s) for the swallowing problem and the best treatment to help
- Identifies if aspiration occurs, this is when food or liquid enters the lungs, and ways to improve the swallowing
- Records the swallowing events to be reviewed after the test
What should I expect?
- The VFSS can be completed on infants, children and adults.
- For adults, no special preparation is typically necessary for this swallowing study. Adult patients do not have to refrain from eating or drinking prior to the test and should take all regularly scheduled medications.
- It is best for infants and young children to be hungry and not eat for several hours before the exam.
- We will first complete an interview before the study to gather medical information and plan the examination.
- During the exam, the patient sits in a special chair and/or stands next to the x-ray machine and drinks liquid and eats foods that are mixed with barium, such as pudding and a cookie. Barium is a contrast agent that lets us see the food and liquid while you swallow, from the mouth through the throat and on its way to the stomach.
- Barium is given to infants/children by bottle or toddler cup depending on the age of the child. Barium is not dangerous for babies or young children. Flavoring can be added to improve the barium taste. The barium may be noticeable in the baby's diaper for a few days after the study.
- During the xray study, various head positions, food textures, and/or bottle types may be tried to see if this improves how you swallow.
- Following the test, the SLP will review the preliminary findings with the patient and family. Once the images are reviewed, a report of the findings is placed within the electronic medical record. The findings are also provided to the referring physician and discussed collaboratively to make recommendations.
Fiberoptic Endoscopic Evaluation of Swallowing (FEES)
FEES is used to assess patients with suspected difficulty swallowing and when there is concern for decreased airway protection during swallowing. It can be performed in a hospital room and/or in our office. Some additional names used for this test are:
- Endoscopy
- Endoscopic Evaluation of Swallowing
- FEES
What is a FEES?
- A very thin, flexible tube, called an endoscope, is inserted gently into the nostril to view the throat and the larynx (the voice box) while eating and drinking
- Looks at the safety of swallowing different types of food and liquid
- Looks at the appearance of the throat and larynx, presence of saliva, and movement of these structures before and after swallowing occurs
- Helps determine the reason (s) for the swallowing problem and the best treatment to help
- Identifies if aspiration occurs, this is when food or liquid enters the lungs, and ways to improve the swallowing
- Records the swallowing events to be reviewed after the test
What to expect?
- The test may be done in the hospital room or in the office or clinic as an outpatient. The test can be done with a patient sitting upright in the hospital bed, in a wheelchair, or in a regular chair.
- This exam lasts about 15 minutes but patients should prepare for an hour-long visit as we collect history information and provide the results and recommendations when the examination is completed.
- All food and liquid is dyed using food coloring, such as blue, to make it easier to see as you swallow
- The endoscope tube has a camera and light on the end and connects to a computer and video monitor for viewing and recording.
- Following the test, the SLP will review the preliminary findings with the patient and family. Once the images are reviewed, a report of the findings is placed within the electronic medical record. The findings are also provided to the referring physician and discussed collaboratively to make recommendations.
Velopharyngeal Insufficiency Study (VPI)
Velopharyngeal insufficiency occurs when the passage between the back of the mouth and the nose (the velopharynx) does not completely close and too much air leaks out of the nose when speaking or swallowing. VPI can occur because of a structural problem, such as in cleft palate, cancer of the palate, or a muscular problem, such as a stroke, cerebral palsy or neuromuscular disorder that causes a weakness or reduced movement of the soft palate/throat. Velopharyngeal dysfunction can cause the following speech characteristics:
- Hypernasality, or too much sound in the nose during speech
- Nasal emission of air
- Short utterance length due to the loss of air pressure through the nasal cavity
What is a VPI study?
- A VPI radiographic study takes place in the radiology department along with the SLP and radiology staff.
- Assesses certain speech sounds for nasal air emission or hypernasality.
- Evaluates the movement of the muscles for speech to help determine why someone may be experiencing nasal speech.
- Determines how severe this speech problem is and guides appropriate treatment.
What to expect?
- The VPI study can be completed on children (ages 4 and up) and adults.
- Barium contrast is placed into the nose via nose drops.
- During the exam, the patient sits in a special chair and/or stands next to the x-ray machine and says various sounds, words, or sentences while an xray video takes images of the nose, mouth and back of the throat.
- We will first complete an interview before the study to gather medical information and plan the examination.
- Following the test, the SLP will review the preliminary findings with the patient and family. Once the images are reviewed, a report of the findings is placed within the electronic medical record. The findings are also provided to the referring physician and discussed collaboratively to make recommendations.
- Sometimes, there are other tests that take place at the same time. This may include a videofluoroscopic swallowing study and/or a speech evaluation and a nasometer to take sound measurements while the patient produces speech.
#1 Research Hospital in America
Mass General is recognized as a top hospital on the U.S. News Best Hospitals Honor Roll for 2023-2024.
