Tumors, cysts, and other types of lesions of the kidney are common among people who have tuberous sclerosis complex (TSC). In fact, kidney problems are the third most common manifestation of the disorder, after brain and skin lesions. Although many kidney abnormalities cause no symptoms, some have debilitating effects on kidney function and on the lives of people who have them.
The two most common kidney, or renal, manifestations in people with TSC are angiomyolipomas (AMLs) and renal cysts. Together these two types of lesions affect 80 percent or more of individuals with TSC. In addition, polycystic kidney disease, a related genetic disorder, occurs in 2 to 3 percent of people with TSC, and renal cell carcinoma, although rare, appears to be more common among those with TSC than in the general population.
Diagnosis
Although renal manifestations associated with TSC may arise at any time, in general they occur in children after age five or young adults. Because of their tendency to increase in size and number over time, regular monitoring of these abnormalities is essential to the care of people with TSC.
Renal Manifestations (in order of frequency):
Angiomyolipomas
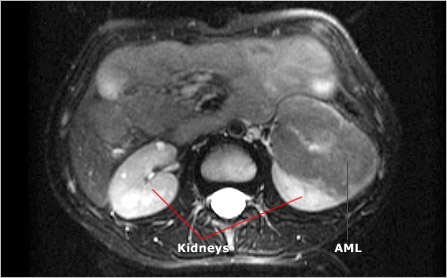
Angiomyolipomas (AMLs) occur in 70 to 80 percent of adults with TSC. These generally benign tumors may occur in children as young as two years old, but most often arise after age five. The name of these tumors refers to their composition: an abnormal collection of blood vessels (angio), smooth muscle (myo), and fat (lipoma). Most people with TSC develop multiple AMLs in both kidneys. In cases where AMLs remain relatively small (less than 4 cm in diameter), they generally cause few problems. Large tumors, however, can negatively affect kidney function by crowding and destroying healthy organ tissue. They can also cause internal hemorrhages if blood vessels associated with them rupture. Such internal bleeding can cause pain and, in rare cases, be life threatening if it goes untreated.
Although single AMLs occur in people who don't have TSC, multiple AMLs are considered characteristic of the disorder and are a major feature in the diagnostic criteria for TSC. Most AMLs are benign. However, people with TSC are more likely than those without the disorder to develop malignant kidney tumors. The rate of malignancy among people with TSC is 1 to 2 percent.
Renal Cysts
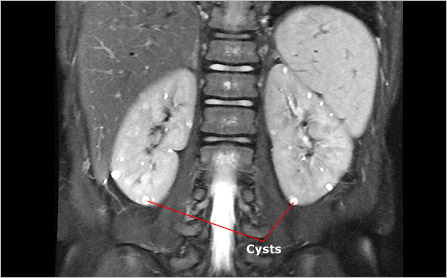
Renal cysts occur in approximately 20 percent of people with TSC. Doctors recognize two types of renal cysts. The more common of the two typically remains small (2 mm to 1 cm in diameter), appears as a single cyst or in small numbers, and has little effect on kidney function. The second type, which affects 2 to 3 percent of people with TSC, is large (1 cm to 5 cm in diameter), often occurs in large numbers, and typically affects both kidneys. This condition is similar to a disorder called polycystic kidney disease and results from a particular type of TSC mutation. In this case, a large portion of DNA on chromosome 16 is altered or deleted, affecting both the TSC2 gene and an adjacent gene called the polycystic kidney disease (PKD1) gene. People who have this condition tend to develop many cysts that grow and ultimately crowd renal tissue and compromise kidney function. Because renal cysts can occur in people with polycystic kidney disease who do not have TSC, they are considered a minor feature in the diagnostic criteria for TSC.
Renal Cell Carcinoma
Studies suggest that people with TSC may carry a slightly higher risk than those without TSC of developing a rare type of cancer called renal cell carcinoma. This cancer, the most common type of kidney cancer in adults, grows in the lining of very small tubes, or tubules, inside the kidney. Because renal cell carcinomas are particularly aggressive, it is important to identify and remove them as early as possible. Unfortunately, the presence of other TSC-related tumors, including AMLs and renal cysts, can make accurate identification of malignant tumors difficult. Physicians may use more than one type of imaging technology (for example, ultrasound or MRI) to identify or rule out the presence of a renal cell carcinoma.
Follow-up and Treatment
Many people with TSC live healthy lives with few complications from the disorder's renal manifestations. However, because of the risks these abnormalities pose, and because kidney lesions can progress rapidly, it is important for people with TSC to undergo regular renal examinations. Aggressive treatments can be very effective in combating the debilitating effects of TSC, but only if problems are identified early in their development.
Specialists recommend that people with TSC undergo renal examinations every two to three years prior to puberty and every year after that. Because large lesions (greater than 4 cm in diameter) tend to grow faster than small lesions and pose a higher risk of hemorrhage, a person with such a lesion may require more frequent examinations.
Physicians and radiologists typically use ultrasound imaging equipment to examine the kidneys of people with TSC. They may also use computed tomography (CT) scans or magnetic resonance imaging (MRI) in cases where higher resolution images are required to determine, for example, whether a lesion is benign or malignant.
For most people with TSC, regular kidney examinations are all that is required to ensure renal health. However, in cases where TSC-related abnormalities affect kidney function more significantly, other steps may be required.
Doctors commonly prescribe antihypertensive medications to help control blood pressure. Controlling blood pressure is particularly important in patients with impaired kidney function. Low-protein diets may play a role as well, minimizing the amount of work an already taxed renal system has to perform.
Doctors may also attempt to slow or stop the growth of progressive kidney lesions, while preserving existing kidney function. One way to do this is through a process called selective embolization. This involves cutting off the flow of blood that feeds a growing tumor, causing the tumor to regress. In cases where embolization is impossible or ineffective, it is sometimes necessary to remove part or all of a kidney to stop the progression of renal tumors.
Next Steps
It is important to remember:
- Many kidney manifestations of TSC have no adverse effects on kidney function, but some do, and their effects can be life threatening
- Angiomyolipomas (AMLs) are benign tumors of the kidney
- Renal cell carcinomas are malignant tumors of the kidney that may be more prevalent in people with TSC than in people without TSC
- Renal cysts are typically small and few in number
- Large, numerous renal cysts suggest a more serious condition: polycystic kidney disease
- TSC specialists recommend kidney screenings every two to three years before puberty and annually after puberty
- Make sure your physician is familiar with TSC-related kidney abnormalities
- Make sure your physician has access to radiologists experienced in distinguishing between benign and malignant renal lesions
- Though it is uncommon, some people with TSC who develop progressive kidney failure may require regular dialysis treatments to make up for their loss of kidney function. This process cleans toxins from the blood that the damaged or missing kidneys would normally remove. For people with such severe kidney dysfunction, transplantation offers the only alternative to dialysis. Physicians have found kidney transplantation to be a useful option in a select group of patients
Tuberous Sclerosis Complex Glossary
Explanations of common terms you'll encounter when learning about TSC.
Patient Gateway
Secure online access to your health information whenever you need it. Check appointments, communicate with your provider and pay bills online 24/7.
Make a Difference for the Herscot Center
Your support is vital to our progress as we move forward into the next generation of teaching, research and clinical care.
