History of Urology at Massachusetts General Hospital
Early History of Mass General
As the population in Boston steadily increased throughout the eighteenth century, the need to provide care for the indigent of the area became increasingly apparent. Although many appreciated the need and some even bequeathed sums to erect a smallpox hospital and a hospital for the insane in Boston, nothing further was done until August of 1810. At that time, two physicians - Drs. James Jackson and John Warren - were sought to remedy the situation by circulating a letter to "some of our wealthiest and most influential citizens for the purpose of awakening in their minds an interest in this subject."

Support for the establishment of a hospital grew. On the 25th of February 1811, a charter for the hospital was obtained from the legislature. It incorporated 56 distinguished inhabitants of various towns of the Commonwealth and was given the power to "hold real and personal estate of the yearly value of $30,000." [1] It was named The Massachusetts General Hospital. The Governor, Lieutenant Governor, President of the Senate, Speaker of the House and the chaplains of both houses constituted the Board of Visitors. The charter imposed on the corporation an obligation to support 30 of the sick and insane persons chargeable to the Commonwealth. Because that mandate would make the institution a pauper house, it was considered disadvantageous and was repealed on February 12, 1816. [2]
The War of 1812 delayed the fund-raising efforts for the construction of the hospital. After the conclusion of the war, prosperity returned to Boston and, in 1817, a fund-raising drive was begun. By March 1817, over $107,000 had been collected.[3] With money in hand, the noted architect Charles Bulfinch was commissioned to design the building. In 1817, a resolution was passed that provided that convicts in the state prison would hammer and fit the stone to be used in the erection of the hospital. Drs. Jackson and Warren were designated as the physician and surgeon, respectively, of the hospital. With all the preparations in order, construction was begun. On July 4, 1818, the cornerstone was laid. The building was opened for patients three years later in 1821. [3]
Development of the Urology Service
When the hospital opened there was no Urology Service per se. During the early years, genito-urinary surgery was treated as part of general surgery with outpatient general surgeons assigned to the care of male patients. Several physicians however, took a special interest in urologic disease and contributed significantly to the advancement of the specialty. Among the physicians who were identified as having an interest in this area at that time were Drs. Henry J. Bigelow and Arthur T. Cabot. [4] Dr. Bigelow contributed significantly to the care of patients with vesicle calculi when, in 1878, he introduced instruments for crushing the calculi and the means to irrigate the fragments from the bladder.
Arthur Tracy Cabot, a renowned MGH surgeon, also made major contributions to the development of the specialty of urology. His interest in genito-urinary surgery and his desire to advance knowledge in the area was apparent when in 1886 he became one of the 22 founding members of the American Association of Genito-Urinary Surgeons. This group consisted of "surgeons known especially for genito-urinary work or who have done good service in the field." [5] The group was formed to exchange information and advance knowledge in the discipline. In 1882, Dr Cabot was elected President of the association. Two years before, he had been appointed Instructor in Genito-Urinary Surgery at Harvard Medical School, the first such mention of the newly emerging field by the medical school.
At the second meeting of the American Association of Genito-Urinary Surgeons, Arthur Cabot addressed the newly formed group with a paper entitled, "A Case of Bowel Ending in the Urethra of a Child Four Weeks Old: Relief by Operation." Because it was the first paper of a disease of childhood presented to this group, this could be considered the beginning of the leadership role played by the MGH in Pediatric Urology." [6]
Arthur Cabot trained many surgeons at the hospital in the specific features of urology of the day. His chief accomplishment was to serve as mentor to his young cousin, Hugh Cabot, who would play a pivotal role in establishing urology as a discipline at the MGH. This influence was acknowledged by the younger Cabot, who dedicated his two volumes, Modern Urology, published in 1918, to "The memory of Arthur Tracy Cabot to whose skill and integrity as a surgeon and to whose wisdom, gentleness and force of character, I desire to express my debt and gratitude." [7]
In the latter half of the nineteenth century, the physicians of the Massachusetts General Hospital organized so that they could speak as one voice to the administration in an attempt to improve conditions. In January of 1898, this group sent a communication to the trustees in which, among other things, it was stated that there was a need for "better accommodations for the Genito-Urinary Clinic, which at present is conducted in two closets. This Genito-Urinary part of the men's surgical room is the largest clinic of its kind in Boston." [8] Very little happened: male patients continued to be seen by physicians assigned from the Surgical Service.
In 1909, the first discussion of establishing a Genito-Urinary Service was recorded. In a letter to the Visiting Surgeons Committee, Dr. Hugh Cabot suggested that such a service be established.
On June 10th, 1910, the trustees voted to establish a Genito-Urinary Service in the Outpatient Department of the Massachusetts General Hospital. Shortly after, on July 22, 1910, Dr. Hugh Cabot was appointed as the surgeon in charge of the Genito-Urinary Department. [9]
Urology Service 1911-1920
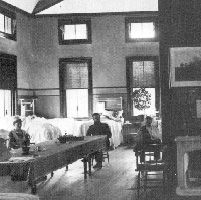
Dr. Cabot expanded the service and gave it an identity. In 1911, the Urology Service was given the use of five beds on the East Surgical Service and five beds on the West Surgical Service - a significant advancement for the Urology Service. The first patient of the Genito-Urinary Service was admitted for treatment of a urethral stricture under the care of Dr. Hugh Cabot. [10]

The head of the Genito-Urinary Department was designated at this point Chief of the Genito-Urinary Service. In 1912, the Genito-Urinary Department was authorized and given a room on the first floor of the outpatient building, initially for men only. Later, females were transferred to it from the female medical and surgical departments. Beds at this time, as noted above, were on the general surgical wards. In 1913, the staff of the Genito-Urinary Service included the Chief of Genito-Urinary Surgery, Dr. Hugh Cabot; genito-urinary surgeons to outpatients, Doctors J. Dellinger Barney, George Gilbert Smith and Richard F. O'Neill; and assistant genito-urinary surgeon to outpatients, Dr. Edward L. Young. During this year, Dr. E. Granville Crabtree received a one-year appointment as the first house surgeon for the Genito-Urinary Service. In 1914, Dr. Crabtree completed the first residency in Genito-Urinary Surgery at the Massachusetts General Hospital.
On November 19, 1914, a bulletin was sent out announcing that female patients could be admitted directly from the Outpatient Department to the Genito-Urinary Service. At this time physicians were instructed that cases of acute gonorrhea were to be transferred to the Genito-Urinary Service and all cases of gangrenous periurethritis were to be admitted to the service and assigned to Dr. J. Dellinger Barney. Another landmark in the development of the Urology Service at the Massachusetts General Hospital occurred in 1916 when the Genito-Urinary Department obtained its own designated beds. These were located on Ward A for men and Ward E for women. [11]
World War I had been raging in Europe when the United States became involved in 1917. Dr. Hugh Cabot, then Chief of the Service, left for France with the Harvard Unit. Dr. O'Neill became the Acting Chief for approximately six months when, in June 1917, he too left for Europe to serve in the armed forces. Dr. George Gilbert Smith was appointed Acting Chief, but he soon left for the army and was replaced by Dr. J. Dellinger Barney until the end of the war and the return of Dr. Cabot. In 1920, Hugh Cabot resigned to become Dean and Chief Surgeon at the University of Michigan. Dr. J. Dellinger Barney was appointed to succeed him. [12]
Urology Service 1920-1969
The Urology Service grew steadily as new technologies were applied to the field and collaborative efforts among specialties developed. In 1925, an x-ray machine was installed in the Phillips House for Urology. Because the need for an interdisciplinary approach to the treatment of stone disease had become apparent, a stone clinic was established about this time as well. Drs. Fuller Albright and J. Dellinger Barney were instrumental in establishing this clinic, with Dr. Albright being placed in charge. This was one of the first combined efforts by physicians, chemists and urologists to manage a disease process. Drs. Richard Chute and Sylvester B. Kelley assisted in the stone clinic. [13]
In 1928, the third floor of the Clinics Building was given to Urology when the Laryngology Service vacated the space and moved to the Massachusetts Eye and Ear Infirmary. This was a major landmark for the service because it made expansion possible. In the clinic, a room for cystoscopies, x-ray examinations and a darkroom were provided. In 1929, the inpatient service census was approximately 25 patients.
Records show that in 1935, the Surgical Executive Committee was established consisting of General Surgery, Orthopedics, Urology and Neurosurgery. [14]Thus, from its inception, Urology played a dominant role in the Surgical Service at the Massachusetts General Hospital. On February 1, 1938, Dr. George Gilbert Smith succeeded Dr. Barry as Chief. He remained in that position until 1945.
In 1939, the White Building opened and Urology was assigned beds on the tenth floor. The floor number was changed to 11 in 1990 to be consistent with the floors of the newly constructed Ellison Building. (This 23-story building was constructed on the footprint of the former Baker Memorial Building.) In 1941, a grant from the U.S. Public Health Genito-Infectious Disease Program helped renovate the Urology Outpatient Department, which was in dire need of updating. As a part of the program, an evening clinic was established for the care of patients with syphilis. [15] Evening hours meant that those patients would not have to miss work.
It became increasingly apparent that some diseases required a multidisciplinary approach. This fact had been recognized years before in the area of stone disease. At this time, such a need was thought necessary for the care of paraplegic patients. Accordingly, White 8 opened as a paraplegic service and became the joint responsibility of the departments of Neurosurgery, Urology, Surgery, Medicine and Orthopedics. [16]
In 1945, Dr. Smith stepped down as Chief of Service and Dr. Fletcher H. Colby was appointed to that position. Under Dr. Colby's direction the Urology Service continued to grow. In 1948, there were 480 admissions to the Urology Ward Service and 441 operations performed. The operative mortality was 3.8 percent. The most common operation was a prostatectomy. Interests of the department included radical cancer surgery, reconstructive surgery of the external genitalia and chemical dissolution of urinary calculi. Drs. Richard Chute and Walter Kerr were instrumental in the first two and Dr. Howard Suby made major contributions to the third. [17]
In the fall of 1954, Dr. Wyland F. Leadbetter was appointed Chief of Urology. During Dr. Leadbetter's years, a strong interest in all aspects of urologic surgery developed at the MGH. His interest in teaching provided for a strong resident service focused on the operative aspects of urology. Many of the residents who received this training went on to become leaders and departmental chairmen in the urologic community.
Pediatric Urology
Several members of the Urology Department were interested in the care of urologic problems of infancy and childhood. Perhaps the first was Arthur Tracy Cabot, but many others contributed as well. While on the faculty, Dr. Victor Poliatano, with Dr. Leadbetter, described a technique for the correction of vesicoureteral reflux. Although significant advances were made by faculty who cared for both adults and children, it wasn't until 1960, when Dr. Hardy Hendren was appointed Chief of Pediatric Surgery, that an individual devoted his entire practice to the care of children.
During his years at the Massachusetts General Hospital, Dr. Hendren, with Drs. Dretler and Leadbetter, established the concept of urinary undiversion, a concept that continues to dominate pediatric and adult urology. He described methods for cloacal reconstruction and the correction of megaureter and expanded the definition of posterior urethral valves. With Dr. Hendren's arrival, ORs 9 and 10 in the Baker Building, which had been delivery rooms, were assigned to Pediatric Surgery. There were no screens on the operating room windows and occasionally pigeon feathers were noted floating across the room. There were no doors in the operating rooms and people walked in an out at will. When the new operating rooms were opened in the Gray Building, Room 31 was assigned to Pediatric Surgery, considerably improving the operating environment. During these early years, Dr. Leadbetter was exceedingly supportive of Pediatric Urology and helpful to its development. Both he and Dr. Hendren developed the concept of Pediatric Urology as a specialty. Through Dr. Leadbetter's efforts, a urology resident was assigned to Pediatric Urology. This began with Dr. Tony Middleton and included all Urology residents who followed him until Dr. Hendren moved to Children's Hospital in Boston. Before leaving the MGH, Dr. Hendren established a fellowship in Pediatric Urology. The first individual to receive the fellowship was Dr. Michael Mitchell, followed by Drs. Terry Hensle and Kenny Crooks. In 1985, Dr. Hendren was appointed the Robert E. Gross Professor of Surgery and Chief of Surgery at Children's Hospital. With his departure from the MGH, the specialty of Pediatric Urology was continued by Drs. Samuel Kim and Patricia Donahoe of the Pediatric Surgical Department.
Urology Service 1969 - Present
Upon the retirement of Dr. Leadbetter, George R. Prout, Jr., MD was appointed Chief of Urology in September 1969. Under the leadership of Dr. Prout, the clinical service continued to be very active and basic research in genito-urinary oncology was developed. He secured laboratory space on Edwards 2, hired a full time PhD and established a scientific foundation for residency education at the MGH. Dr. Prout introduced the concept of protocols and randomization to the Urology Service. During his tenure, an interdisciplinary approach to oncology was emphasized, combining the expertise of radiation, medical and urologic oncologists. Bladder cancer research was significant but not to the exclusion of other areas of urologic oncology. Many international fellows rotated through the laboratory - a tradition that continues to this day. Dr. Prout was also instrumental in expanding the role of the attending surgeon in surgical education in the operating room.
As the Urology Service expanded, private Urology patients were located on White 9 (originally White 8), the Phillips House and the Baker Building. White 11, the designated urology floor since the opening of the White Building, housed the service patients. Endoscopic procedures were performed on White 11 until 1975 when the endoscopic suite was closed and moved to Warren/Baker 12 for a short period. After that, all inpatient endoscopy procedures were performed in the White operating room.
The academic offices had also been located on White 11 until June 6, 1976. Upon the completion of the Bigelow Building renovations, they were moved to Bigelow 11. White 11 remained the Urology floor until 1994, at which time all Urology patients were moved to Bigelow 11. In 1996, White 11 was reclaimed for Urology.
In 1984, one of the first lithotriptors in the United States was placed at the MGH and located in the x-ray department on White 2. This lithotriptor was the Dornier HM3. In 1992, the Lithotriptor Unit on White 2 was moved to White 3, adjacent to the main operating room, and a new generation lithotriptor, the Dornier MLF-5000, was installed.
The Outpatient Department remained on the third floor of the Clinics Building until 1985. The space was shared with the Genito-Infectious Disease section (GID). In 1985, the clinic was moved to the newly constructed Wang Ambulatory Care Center and placed on the fifth floor. Until this time, all outpatient cystoscopies were done in the main operating room or as transients on White 10. Simple observational cystoscopies could be performed in the clinic, but until 1991 there was no capability for performing more complex endoscopic procedures. In 1991, the clinic space was renovated. A fixed-table x-ray unit was installed so that minor surgical as well as endoscopic procedures requiring local anesthesia could be performed. For the first time, private and service patients were seen in the clinic concurrently.
Upon the retirement of Dr. Prout in 1989, Dr. Niall M. Heney served as Interim Chairman until January 1, 1991, when Dr. W. Scott McDougal was appointed to succeed Dr. Prout.
Under Dr. McDougal's leadership, the concept of subspecialization was introduced. Faculty members were encouraged to devote a major portion of their time to specific domains in urology. The teaching service was enhanced, ambulatory procedures were performed in the clinic and an effort was made to have all faculty at MGH in the full time category.
In 1998 the Urology Laboratory was moved from the Edwards Building to renovated space on Warren 3. The faculty had been expanded to include physicians from pathology who have a special interest in genitourinary tumors. This facilitated the establishment of a GU tumor bank, which is maintained by the Department.
In 1999, Dr. Robert Krane joined the faculty and established the Neuro-urology Division. Dr. Krane had been Chairman of Urology at Boston University and was an international expert in erectile and voiding dysfunction. He added video urodynamics and trained support staff and physicians in neuro-urologic diagnostic techniques. His untimely death in the fall of 2001 was a great loss to the Department; however, the excellence of the Urodynamics Laboratory developed under his leadership continues.
In the fall of 2001, the Department recruited faculty with a special interest in minimally invasive and laparoscopic surgery. Laparoscopic urologic procedures had been performed at the MGH by Drs. McDougal and Dretler since the early 1990's, but the additional faculty allowed for a marked expansion of the area of minimally invasive surgery.
References
1. Bowditch, NI, A History of the Massachusetts General Hospital, privately published, Boston, 1872, p.3.
2. Ibid., p. 10.
3. Faxon, NW, The Massachusetts General Hospital 1935-1955, Harvard University Press, 1959, p.4.
4. Washburn, FA, The Massachusetts General Hospital, Houghton Mifflin Co., Boston, 1939, p. 347.
5. Spence, HM, A History of the American Association of Genito-Urinary Surgeons 1886-1982, published by American Association of Genito-Urinary Surgeons, 1982, p. 6.
6. Ibid., p. 9.
7. Cabot, H, Modern Urology in Original Contributions by American Authors, Lea & Febiger, Philadelphia, 1918.
8. Washburn, op. cit., p. 213.
9. Washburn, op. cit., p. 348.
10. "MGH Hospital Records of the Genito-Urinary Service," Volume 1, August 1911.
11. Washburn, op. cit., p. 216.
12. Washburn, op. cit., p. 350.
13. Washburn, op., cit., p. 408.
14. Faxon, op. cit., p. 9-10.
15. Faxon, op. cit., p. 16.
16. Faxon, op. cit., p. 303.
17. Urology Service Report #133, p. 1, April 1954.
Biography References
Hugh Cabot
Spence, HM, "Hugh Cabot: Founder of the Urological Service at the Massachusetts General Hospital," Transactions American Association of Genito-Urinary Surgeons, 1994.
J. Dellinger Barney
Transactions American Association of Genito-Urinary Surgeons
George Gilbert Smith
Transactions American Association of Genito-Urinary Surgeons, Volume 56, 1964.
Fletcher H. Colby
Transactions American Association of Genito-Urinary Surgeons, Volume 59, 1967.
Wyland F. Leadbetter
Transactions American Association of Genito-Urinary Surgeons, Volume 67, 1975.
Appendix A
Chairmen of Urology
Hugh Cabot 1872 - 1945
Hugh Cabot was born in 1872 in Beverly Farms, Massachusetts, a town 20 miles northeast of Boston. He received his secondary education at the Latin School and subsequently matriculated at Harvard. He was elected to Phi Beta Kappa and Sigma XI and was graduated in 1894. Four years later he was granted the MD degree cum laude from Harvard Medical School. Following graduation from medical school, he was appointed to the Surgical Service at the Massachusetts General Hospital as a "House Pupil." During this time he was influenced by his cousin, Dr. Arthur T. Cabot, who had a special interest in diseases of the genito-urinary system. Upon completion of his formal training, he practiced in Boston in association with Arthur Cabot.
Although Hugh Cabot never limited his practice to genito-urinary conditions, he established the Urology Residency at the MGH and in1918, published Modern Urology, one of the first texts devoted entirely to the discipline of Urology.
In 1916, he took a leave of absence from the MGH in order to organize and lead the Harvard Unit to France as part of the British Expeditionary Force during World War I. For these efforts he was awarded Commander of the Order of St. Michael's and St. James by the British Government. When the war was over, he returned to the MGH and resumed his leadership of the Urology Service. In 1918, he was named Clinical Professor of Genito-Urinary Surgery at Harvard Medical School.
In 1920, he left Boston to assume the position of Dean and Professor of Surgery at the University of Michigan Medical School. He built the surgical program at the University of Michigan Medical Center but ultimately was forced to resign because of controversy concerning his autocratic methods. He took a position at the Mayo Clinic where he remained until his retirement. He returned to Boston and died in 1945 of a heart attack.
Dr. Cabot was President of the American Urologic Association in 1911, President of the American Association of Genito-Urinary Surgeons in 1914 and a founding member of the Clinical Society of Genito-Urinary Surgeons as well as the American College of Surgeons.
J. Dellinger Barney 1878 - 1959
James Dellinger Barney was born in Boston in 1878. He attended Harvard College and the Harvard Medical School from which he obtained his MD degree in 1904. He served a surgical internship at the MGH and subsequently remained on the staff. Dr. Barney became interested in the specialty of urology and joined the Department of Urology when it was established in 1911. He became Chief of Urology in 1920 and Assistant Professor of Surgery at Harvard. He retired as Chief at the age of 60 but continued in private practice in Boston until 1950 when he retired completely. He died in 1959 at the age of 81.
Dr. Barney belonged to the American College of Surgeons and the American Urological Association. He served as President of the American Association of Genito-Urinary Surgeons in 1936 and was a member of the Clinical Society of Genito-Urinary Surgeons.
George Gilbert Smith 1883-1963
George Gilbert Smith was born in Brooklyn, New York on September 23, 1883. He received an AB degree from Harvard College in 1905 and an MD degree from Harvard Medical School in 1908. He was an intern at the MGH from1908 to 1909 after which he entered private practice in Boston. An early interest in urology led him to his appointment to the urological staff of the MH in 1912. The development of the Urology Service and its postgraduate program became his primary interests. Dr. Smith was appointed Lecturer in Surgery at the Harvard Medical School from 1940 to 1945. In 1919, he authored a urologic text entitled Outline of Genito-Urinary Surgery. His contributions to the area of prostate cancer were numerous.
Dr. Smith was a diplomat of the American Board of Urology and was a trustee of the Board from 1937 to 1953. In addition, he was a fellow of the American College of Surgeons, President of the American Urological Association 1935 to 1936, President of the American Association of Genito-Urinary Surgeons 1938 to 1939, President of the Clinical Society of Genito-Urinary Surgeons 1944 to 1945 and President of the Societe Internationale d'urologie from 1947 to 1955. He was made an honorary member of the British Association of Urologic Surgeons.
Fletcher H. Colby 1893 - 1966
Fletcher H. Colby was born in Berlin, New Hampshire in 1893. After graduating from Phillips Exeter Academy, he received his AB degree from Dartmouth College. In 1918, he was granted his medical degree from Harvard Medical School. He served in the Navy's medical corps during World War I and then returned to Boston where he interned at the MGH from 1919 to 1921. He became a resident in Urology at the Peter Bent Brigham Hospital under Dr. William Quimby. Following his residency, he practiced Urology with Dr. George G. Smith. Dr. Colby was Associate Clinical Professor of Surgery at Harvard Medical School and from 1945 to 1954 he served as Chief of Urology at the MGH.
He was President of the New England section of the American Urologic Association in 1937, President of the American Association of Genito-Urinary Surgeons in 1955, President of the Clinical Society of Genito-Urinary Surgeons in 1955, and a member of the American College of Surgeons.
He wrote extensively and is best known for his Essential Urology, a text for medical students, and Pyelonephritis. He died on August 14, 1966.
Wyland F. Leadbetter 1907 - 1974
Wyland F. Leadbetter was born in Livermore Falls, Maine on January 9, 1907. After graduation from high school, he attended Bates College where he later became a trustee. He then went to Johns Hopkins Medical School and graduated in 1932. At Bates College he was elected to Phi Beta Kappa and at Johns Hopkins Medical School he was elected Alpha Omega Alpha Honorary Society. His surgical and urologic residencies were at Johns Hopkins University Hospital from 1932 to 1938 under Dr. Hugh Young.
After his residency, he practiced for a short time at the Lahey Clinic. He then entered the army in 1942 as a member of the 33rd General Hospital and served overseas during the African campaign and the invasion of Sicily. After World War II, he was in private practice briefly before being appointed Professor of Urology at Tufts Medical School and New England Medical Center Hospital. He served in that position from 1947 to 1954 and then was appointed Clinical Professor of Surgery at Harvard Medical School and Chief of Urology at the Massachusetts General Hospital.
During his 36 years of urologic practice, he was a member of many societies, which have influenced the standard of teaching of urology. Some of these include the American Medical Association, American College of Surgeons, Societe Internationale d'Urologie, American Academy of Pediatrics, Society of Pediatric Urology, American Association of Genito-Urinary Surgeons, Clinical Society of Genito-Urinary Surgeons and the American Urological Association. He was Secretary and President of the New England section of the American Urologic Association and during his last seven years he was Secretary and President of the American Urologic Association. In 1970, he served as President of the Clinical Society of Genitor-Urinary Surgeons and in 1974 as President of the American Association of Genitor-Urinary Surgeons. In addition, he was a diplomat of the American Board of Urology and a trustee of the Board from 1957 to 1965. Dr. Leadbetter died on August 28, 1974.
George R. Prout, Jr. 1924 - 2013
George Prout, Jr. was born in Boston, Massachusetts on July 23, 1924. His family subsequently moved to Dallas, Texas where he grew up. He attended Union College and received his medical degree from Albany Medical School in 1947. At that time he was elected to the Alpha Omega Alpha Honorary Society. His urologic training was at Cornell-New York Hospital under Dr. Victor Marshall and at Memorial Sloan-Kettering Cancer Center under Dr. Willet Whitmore.
When his training was completed, he assumed the position of Chief of Urology at the University of Miami. In 1960, he was appointed Chairman of Urology at the Medical College of Virginia. There he worked closely with Dr. David M. Hume, a pioneer in renal transplantation. In 1969, he was appointed Professor of Surgery at Harvard Medical School and Chief of Urology at the Massachusetts General Hospital. Dr. Prout was a true academician - an excellent teacher, a scientist and a respected clinician. He made many fundamental contributions in the area of urologic oncology and was responsible for enhancing the scientific foundation of the Residency Program in Urology at the MGH.
He retired in 1989. He is a member of the American Urologic Association, the American College of Surgeons, the American Association of Genito-Urinary Surgeons and a diplomat of the American Board of Urology.
W. Scott McDougal 1942 -
W. Scott McDougal was born in Grand Rapids, Michigan on July 11, 1942. He received his AB degree from Dartmouth College in 1964 and his MD degree from Cornell Medical College in 1968. He took his postgraduate surgical training at University Hospitals in Cleveland - Case Western Reserve University Medical School where he was appointed jointly to the departments of General Surgery and Urology. He completed his general surgical residency under Dr. William D. Holden and his urological residency under Dr. Lester Persky. During this period, he spent a year as a postdoctoral fellow in renal physiology at Yale Medical School. Following residency training, he was inducted into the army and assigned as a general surgeon to the Institute of Surgical Research at Brooke Army Medical Center where he was Chief of the Burn Study Branch.
Following discharge from the military, he returned briefly to the University Hospitals of Cleveland before assuming the chairmanship of Urology at Dartmouth Medical School. In 1984, he was appointed Chairman and Professor of Urology at Vanderbilt Medical School where he remained until January 1991. At that time he was appointed Chief of Urology at the MGH and Professor of Surgery at Harvard Medical School. On March 11, 1996, he was named the Walter S. Kerr, Jr., Professor of Urology at Harvard Medical School.
He is a diplomat of the American Board of Surgery, a diplomat of the American Board of Urology, a trustee of the American Board of Urology from 1990 to 1996 and its President from 1995 to 1996, a member of the American Association of Genito-Urinary Surgeons, the Clinical Society of Genito-Urinary Surgeons and a fellow of the American College of Surgeons.
Dr. Michael L. Blute received his BA Degree from the College of the Holy Cross in Worcester, and his medical degree from Creighton University School of Medicine in 1982, graduating Magna Cum Laude. Subsequent to internship and residency in urology at the Mayo Clinic in Rochester, he remained on the staff and rose rapidly through the ranks to become the Anson L. Clark Professor and Chairman in the Department of Urology in 1999. He remained as Chairman of the Department of Urology and on the Executive Board of the Mayo Clinic until appointed Interim Chief of Urology and Director of the Cancer Center of Excellence at the University of Massachusetts Memorial Medical Center in 2010. In April 2012 Dr. Blute was appointed Chief of Urology at The Massachusetts General Hospital in Boston and is the Walter S. Kerr, Jr. Professor of Surgery, Harvard Medical School.
Dr. Blute has had a major interest in urologic oncology and is well-known in the field of academic urology. His major areas of interest include prostate cancer, nephron-sparing surgery for kidney masses and the management of complex renal cell and bladder neoplasms. He has been involved in phase III trials of Finasteride, chemoprevention of prostatic intraepithelial neoplasia with anti-androgens, minimally invasive surgery for BPH, biomarkers in prostate cancer, and discovery of B7 family of “Check Point Inhibitor” Biomarkers in kidney cancer.
He serves as a reviewer on 13 editorial boards. He also serves on the AUA Renal Mass Guideline Panel and the American Joint Committee on Cancer. He was the recipient of the 2010 AUA Career Contribution Award. His bibliography includes 387 peer-reviewed publications, one book and 26 book chapters.
View a listing of the graduates from the Harvard Urologic Surgery Residency Program.
Mass General Urology
We provide sophisticated, compassionate care and the most innovative treatments for patients with any type of urological condition.
