What is FND?
Functional neurological disorder (FND) is a problem largely impacting the function of the brain. It is considered a condition directly at the intersection of neurology and psychiatry – also known as a ‘neuropsychiatric’ disorder. In FND, the normal pathways your brain uses to move, feel, speak, walk, and/or think, are disrupted. This promotes symptoms such as paralysis (not being able to move part of the body), episodes that resemble seizures, extra movements such as tremor or jerks, problems with memory, etc.Are there other names/terminology for FND?
Functional neurological disorder, or FND for short, is the preferred terminology by many experts in the field, because it does not imply a specific cause for symptoms and takes into account that different people can have FND for different reasons. FND is still referred to sometimes as "conversion disorder." Because FND is likely not caused by a single mechanism across all patients (and because risk factors also vary across patients), "conversion disorder" has fallen out of favor with many experts.Additional terms that have been used to describe FND symptoms in the past include hysteria, medically unexplained symptoms, psychogenic, psychosomatic and non-organic. We no longer use these terms for a variety of reasons. For example, many patients and care providers found these terms offensive. ‘Medically unexplained’ isn’t accurate because we understand some of the brain mechanisms that lead to FND.
What types of symptoms can FND cause?
FND can look different depending on the person. Below is a list of some common symptoms. This list is not exhaustive, and someone with FND may only have one or two symptoms on this list. Having FND does not mean that you will get all of these symptoms.- Weakness
- Seizure-like events
- Tremors or jerks
- Walking problems
- Memory or thinking difficulties
- Speech symptoms
What goes wrong in FND?
In FND, the normal pathways your brain uses to do things such as move, feel, speak, walk, or think, get disrupted. One analogy we often use is to compare FND to a software problem of your brain. If you think of your brain as a computer, it’s like one of the programs on that computer isn’t working properly (for example, the program for how to walk) or in some cases like the computer is crashing (like with functional seizures). The hardware, or structure of the brain, is normal (as an aside, an example of a hardware problem of the brain would be something like a stroke or multiple sclerosis). Another way of conceptualizing FND is that different brain areas are having difficulties communicating with one another – leading to a range of motor and sensory symptoms.What causes FND?
We are still learning why some people get FND, while others do not. FND is a disorder that has biological, psychological, and social risk factors and events that trigger it. The ‘equation’ for the relevance of given biological, psychological and social factors varies across patients.How is FND diagnosed?
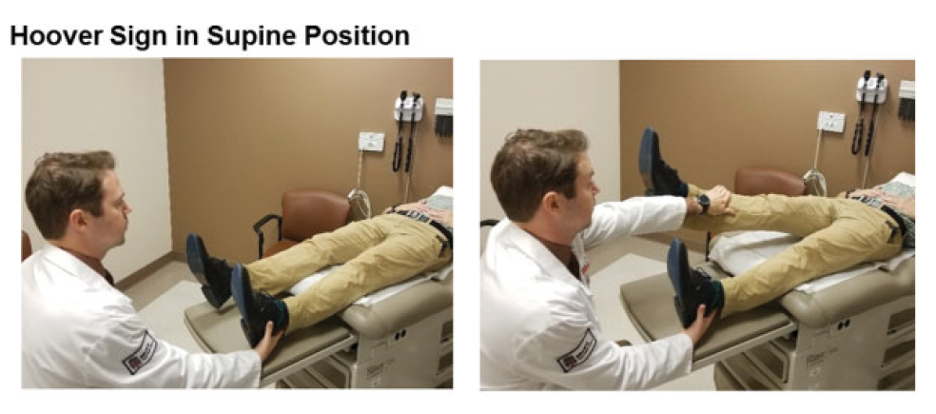
FND should typically be diagnosed by a neurologist or neuropsychiatrist, both of whom specialize in disorders of the brain. Your doctor will use neurological examination expertise to check for the presence of positive clinical signs, such as a Hoover’s sign, that are consistent with FND in order to make the diagnosis. In the case of functional seizures, your doctor will try to observe an event (either in person or captured on video) and look for positive clinical signs during the event.Diagnosis of FND is not based on the fact that you are stressed or that you have a history of depression, anxiety, or other mental health diagnosis.
Reference: Functional (Psychogenic) Neurological Disorders: Assessment and Acute Management in the Emergency Department. Anderson JR, Nakhate V, Stephen CD, Perez DL. Semin Neurol. 2019 Feb;39(1):102-114. doi: 10.1055/s-0038-1676844
Are there tests that can confirm I have FND?
FND is a clinical diagnosis – which means that we make the diagnosis based on a physical examination or, in the case of functional seizures, getting a detailed description of the events along with brain wave (EEG) data in some instances. Many disorders have a clinical diagnosis, including Parkinson disease or major depressive disorder. There are no specific tests to confirm that you have FND. In fact, we expect testing we get done to be generally normal. This is because most testing we have available checks for structural problems of the nervous system, as opposed to problems of nervous system function.
How is it treated?
FND symptoms are potentially reversible. However there are generally no quick fixes. Treatment focuses on teaching you how to retrain your brain – helping you bring your movements, speech, thinking, or other neurological symptoms back to normal function. Treatment depends on the FND symptoms you have and is often ‘multidisciplinary.’ This means that care providers from different specialties, like physical therapy and social work/psychology, can often times be involved in patient care. For a patient who is mainly having problems with movement, we may suggest physical therapy to retrain your movement. For a patient with functional seizures, we may suggest seeing a psychotherapist for cognitive behavioral therapy, to help you learn how to manage and in some cases prevent these events. Because FND is a complex problem, sometimes with complex treatments, you, as the patient, are an important member of the treatment team. We rely on you to practice the skills you learn with our treatment team, keep an open mind, and let us know what works and what doesn’t.
Is it all in my head?
Sort of, in the sense that your brain is in your head, and this is a problem of brain function. What is important to know is that FND is a REAL brain-based problem – it is not something you are imagining, making up, or bringing on yourself. It is also not the same thing as, or solely caused by, things like stress, anxiety, or depression. Psychological factors can be risk or triggering elements for some individuals, but they are only one part of the overall clinical picture.
If this is a brain problem, why are you recommending psychotherapy as treatment?
First, it is important to understand that neurology and psychiatry have been somewhat artificially separated. They both deal with problems of the brain, but come at it from different perspectives. While FND used to be considered a purely psychological problem, most experts in the field now agree that it is a disorder that sits in between the fields of neurology and psychiatry. Both biological and psychological factors can play a role in making you more likely to get FND or trigger FND symptoms. So, one reason we may recommend psychotherapy as treatment is because for some of our patients it is a big piece of their FND puzzle, and important to address. Psychotherapy can also be thought of as a form of “brain retraining”.
Second, there have been clinical trials with FND patients that show that psychotherapy can be helpful for some patients.
Third, some patients with FND also have significant depression, anxiety, or another mental health disorder that is happening in parallel with their FND. Since these problems can make FND worse, they are important to treat.
Where can I learn more?
One resource is the website www.neurosymptoms.org. This is a website made by Prof. Jon Stone, based out of the UK, who is a world-wide expert in FND. It contains information, videos, and links for both healthcare providers and patients.
Patient Gateway
Secure online access to your health information whenever you need it. Check appointments, communicate with your provider and pay bills online 24/7.
