Mass General Brigham
Sports Medicine Fellowship


Contact Information
Mass General Brigham Sports Medicine Fellowship
Elizabeth Matzkin, MD
Fellowship Director
175 Cambridge Street, Suite 400
Boston,
MA
02114
Phone: 617-643-4796
Fax: 617-643-7908
Email: nalessi@bwh.harvard.edu
Elizabeth Matzkin, MD, Fellowship Director
Eric Berkson, MD, Fellowship Associate Director
Nancy Alessi, MGB Sports Medicine Fellowship Coordinator
nalessi@bwh.harvard.edu
Explore the Sports Medicine Fellowship
The Brigham & Women’s and Mass General Sports Medicine Fellowship programs are merging to create the Mass General Brigham Sports Medicine Fellowship, effective August 1, 2026. For fellowship inquiries for the 2026-2027 academic year and beyond, please contact Nancy Alessi, Program Coordinator, nalessi@bwh.harvard.edu, phone 617-732-9551. For information regarding the 2025-2026 fellowship year, please continue to reach out to Wendy Ames, wames@mgb.org.
Overview
The Mass General Brigham Orthopedic Sports Medicine Fellowship is a one-year program designed to provide mentorship and a learning environment focused on comprehensive clinical training, cutting-edge research and innovative patient care.
We strive to set the gold standard in sports medicine education, research and clinical practice, preparing our fellows to excel in any setting and positively impact the lives of athletes worldwide. The fellowship begins on August 1 and ends on July 31.
Mission
Our mission is to:
- Teach fellows critical thinking skills and practical surgical expertise in treating both routine and complex sports medicine problems.
- Emphasize the roles and responsibilities of a team physician.
- Foster a spirit of scientific inquiry and advancing the field through research and innovation.
- Develop compassionate physician-leaders who will shape the future of sports medicine.
- Deliver exemplary, patient-centered care that optimizes athletic performance and overall wellbeing.
- Promote injury prevention and wellness in our local and global communities.
Educational Program
Core Rotations
Each of our four Fellows will spend two months on each of the four Core Rotations.
1. Hip+
Arthroscopic hip with additional general knee and shoulder sports medicine
- Scott Martin, MD
- Richard Wilk, MD
- Bioskills/Research
2. Shoulder
Arthroscopic and open complex shoulder, including arthroplasty, instability and muscle transfer
- JP Warner, MD
- Ryan Lohre, MD
- Logan Huff, MD/Giovanna Medina, MD, PhD
3. Sports
High volume knee, shoulder repair and reconstruction
- Elizabeth Matzkin, MD
- Robert Nascimento, MD
- Ian Hutchinson, MD/Morgan Jones, MD
4. Knee
Complex knee, cartilage restoration, patellofemoral
- Christian Lattermann, MD
- Eric Berkson, MD
- Miho Tanaka, MD, PhD
Elective Rotations
Each fellow will spend the final 4 months of the fellowship choosing two elective rotations.
Elective rotations
General Sports
- Simon Goertz, MD
- Ian Hutchinson, MD
- Morgan Jones, MD
- Elizabeth Matzkin, MD
- Robert Nascimento
Patellofemoral
- Eric Berkson, MD
- Miho Tanaka, MD
- Christian Lattermann, MD
- Nikolaos Paschos, MD, PhD
Pediatric Sports Medicine
- Giovanna Medina, MD, PhD
- Nikolaos Paschos, MD, PhD
Sports Elbow
- Neal Chen, MD
- Matt Leibman, MD
- Gus Mazzocca, MD
Sports Foot and Ankle
- Jeremy Smith, MD
- George Theodore, MD
- Greg Waryasz, MD
Complex Knee
- Eric Berkson, MD
- Simon Goertz, MD
- Ian Hutchinson, MD
- Christian Lattermann, MD
- Scott Martin, MD
- Elizabeth Maztkin, MD
- Robert Nascimento, MD
- Nikolaos Paschos, MD, PhD
- Lars Richardson, MD
Complex Shoulder
- Arnold Alqueza, MD
- Bassem Elhassan, MD
- Ryan Lohre, MD
- Robert Nascimento, MD
- Evan O’Donnell, MD
- Jon JP Warner, MD
Sports Hip
- Scott Martin, MD
- Nikolaos Paschos, MD, PhD
- Richard Wilk, MD
Shoulder Instability
- Logan Huff, MD
- Morgan Jones, MD
- Elizabeth Matzkin, MD
- Gus Mazzocca, MD
- Robert Nascimento, MD
- Evan O’Donnell, MD
- JP Warner, MD
Research
- Mark Cote, PT, DPT
- Cale Jacobs, PhD, ATC
- Morgan Jones, MD
- Miho Tanaka, MD, PhD
- Christian Latterman, MD, PhD
Women's Sports Medicine
- Elizabeth Matzkin, MD
- Miho Tanaka, MD, PhD
- Giovanna Medina, MD, PhD
Rehab/Performance/MRI
- Eric Berkson, MD
- Christian Lattermann, MD
- Joe Simeone, MD
- Kirstin Small, MD
- Bill Palmer, MD
- Scott Waugh, PT
- David Nolan, PT, DPT

Case Volume
Fellows can expect more that 500 operative cases during fellowship with a high case complexity, focusing on complex knee reconstruction, cartilage restoration, shoulder instability, shoulder arthroplasty, muscle transfers around the shoulder and more. Additional subspeciality sports medicine exposure is available through elective rotations.
Average cases per fellow in select anatomic areas:
- Shoulder arthroscopy: 152
- Knee arthroscopy: 111
- ACL: 73
- Shoulder arthroplasty: 44
- Shoulder tendon transfers: 20
- Complex shoulder instability (Latarjet, Allograft, etc): 18
- Cartilage restoration: 12
- Hip arthroscopy: 10
- Multiligamentous knee reconstruction: 18
- Meniscal transplant: 6
- Lower extremity osteotomy: 8
- Sports elbow: 6
External Meetings
Planned Fellowship support:
- New England Shoulder and Elbow Society (Jay Peak, VT)
- International Sports Medicine Fellows Conference (Carlsbad, CA)
- AOSSM/AANA
- Arthrex, Smith & Nephew, Stryker Sports Medicine Courses
- NFL Combine
- Boston Red Sox Spring Training
Conferences & Didactics
- The MGB Sports Medicine Fellowship sits within the larger framework of MGB Orthopaedics and includes access to MGB Orthopaedic grand rounds, M&M and multidisciplinary educational conferences.
- Sports Medicine Conference (weekly conference attended by fellows and attendings from orthopaedic sports medicine, orthopedic shoulder fellowship, primary care sports medicine, emergency sports medicine, physical therapy). We expect collaborative learning across disciplines within sports medicine and orthopaedic surgery.
- Weekly morning case discussions, sports-specific M&M
- Shoulder indications conference
- Research meetings
Sports Coverage Opportunities

Major coverage responsibilities
- New England Patriots (NFL): Every fellow, 2 months
- Harvard University: Training room, occasional game coverage
- Boston College: Training room, football & hockey coverage
- Stonehill College: Training room, football & hockey game coverage
- Local high schools: Usually assigned one school
Elective coverage
- Boston Red Sox (MLB): All fellows attend Spring Training in Ft. Myers, FL
- Boston Bruins (NHL)
- New England Revolution (MLS)
- Northeastern University: Paid coverage, if interested
- Boston Fleet (PWHL)
Research
The MGB Sports Medicine Fellowship offers the resources of a major academic university-based medical center. MGB Sports Medicine published 370 papers in the last 18 months. Research exposure and experiences can be customized to each fellow. There is ample research time for basic science and clinical projects with support from dedicated Sports Medicine research leadership (Mark Cote, PT, DPT and Cale Jacobs, ATC, PhD), statisticians, Research Assistants, Clinical Orthopaedic Sports Medicine and Outcomes research (COSMOS), BWH Orthopaedic and Arthritis Center for Outcomes research (OrACore) as necessary.
Patient-Related Outcomes Research
- Patient IQ “behind the scenes” data collection
- Starnet Biorepository
Lab-Based Research
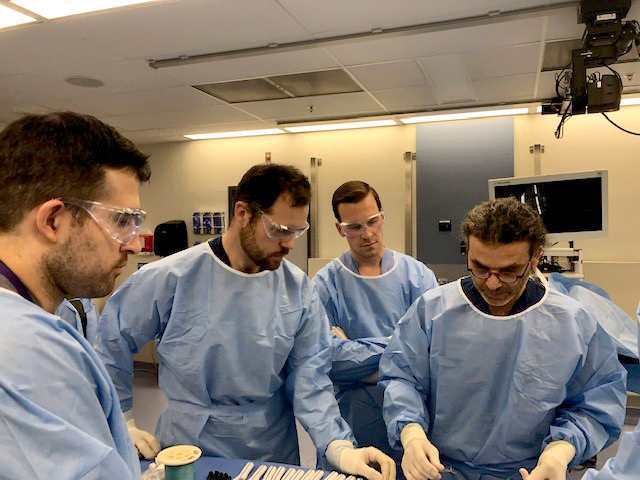
- ENABLE Bioskills Laboratory
- The ENABLE LAB located at the Charlestown Navy Yard which is 4000 square feet dedicated to Sports Medicine Research and General Orthopedics. This has a bioskills lab with six state-of-the-art arthroscopy towers that will allow further training on complex hip arthroscopy (c-arm and cadaver hips), elbow reconstruction, knee osteotomy and ligament reconstructions as well as all other procedures. A dedicated biomechanics lab with Instron machine, Vicon motion analysis cameras and a cadaver shoulder/knee simulator. It will also house a staffed cell biology lab investigating bone to tendon healing and biologic research.
- Lattermann/Charles PTOA Laboratory
- Scott Martin Hip Laboratory
- Center for Sport Performance and Research
- Center for Sports Performance and Research (CSPaR): The Mass General Brigham Center for Sports Performance and Research offers a science-based approach to the training of sport and tactical athletes, conducting innovative research to enhance and sustain athletic performance and aid fast and effective athlete recovery.
Women’s Sports Medicine Research
- Matzkin Research Group
- Tanaka Research Group
Participation in basic science and clinical research projects will be encouraged throughout the year with instruction on study design and preparation, presentation, and manuscript preparation.
Each fellow is required to complete at least one research project during their fellowship year.
Financial support is provided for presentation of research projects at national meetings.
Faculty
Core Faculty
- Elizabeth Matzkin, MD, Fellowship Director
- Eric Berkson, MD, Fellowship Associate Director
- Christian Lattermann, MD
- Ryan Lohre, MD
- Scott Martin, MD
- Augustus Mazzocca, MD
- Robert Nascimento, MD
- JP Warner, MD
- Richard Wilk, MD
Fellows rotate with additional Harvard Medical School faculty within MGB Orthopedic Sports Medicine and have access to elective rotations with MGB Physiatry, MGB Physical Therapy, MGH and Brigham Musculoskeletal Radiology.

How to Apply
- Duration: 1 year (August 1 to July 31)
- 4 fellows are accepted per year
- The applicant must be Board-eligible and obtain a full Massachusetts license
- This fellowship is ACGME accredited
For further information on resources for prospective fellows including salary and benefits, please see the MGB Graduate Medical Education site.
The Mass General Brigham Orthoapedic Sports Medicine Fellowship participates in the SF Match. Applicants can apply on the SF Match website.
Further information on the Sports Fellowship match can be found on the AOSSM website.
Sports Medicine Service
The Sports Medicine Service at Mass General provides custom treatment and rehabilitation plans for injured athletes of all ages and abilities. Get off the sidelines and back into the game with Mass General.
