Pediatric Inflammatory Bowel Disease Center


Contact Information
Pediatric Inflammatory Bowel Disease Center
Yawkey Center for Outpatient Care
55 Fruit Street, Suite 6B
Boston,
MA
02114
Phone: 877-733-4423
Patients may also call the Pediatric GI Call Center at 617-726-8705 to schedule an appointment.
Other Locations
MGfC at Newton Wellesley Hospital Pediatric IBD Program
Newton Wellesley Hospital
6 South
2000 Washington Street
Newton, MA
Medical Infusion Unit
MGH-West
52 Second Avenue, Suite 300
Waltham, MA 02451
Explore This Treatment Program: Ulcerative Colitis and Crohn's Disease
Schedule a Virtual Visit
Our team provides patients with virtual visits using video-based programs over a secure Internet connection to the patient’s desktop computer, laptop or tablet. Virtual visits give our patients and families a direct video link with their doctor without having to travel for an appointment. Patients may discuss symptoms and clarify treatment plans from the comfort of their home or another private setting. To arrange a virtual visit, please call 877-733-4423.
Learn more about virtual visitsOverview
Children with a chronic illness benefit from a multidisciplinary approach to their care. We have built a team with expertise in diagnosing and managing children and adolescents with inflammatory bowel disease (IBD).
Team approach for individual patients
Patients are cared for by an IBD team that includes:
- Pediatric gastroenterologist who specializes in caring for patients with IBD
- Experienced IBD nurse
- Nutritionist
- Psychologist/psychiatrist
- Social worker
- Pediatric surgeon

The Pediatric Inflammatory Bowel Disease team at Mass General for Children. - Radiologists experienced in evaluating IBD
- Pathologists with expertise in diagnosing IBD
These specialists work together in a single program to provide a comprehensive approach to the care of your child. Every patient requires individualized care reflecting this individuality. We strive to incorporate current evidence-based guidelines and ongoing clinical, translational, and basic science research to offer the most up-to-date treatment options for our patients.
Diagnosing IBD
Patient evaluation involves a detailed history and exam. Further testing may include blood testing, endoscopic testing, and radiologic studies. If your child needs a procedure (endoscopy or radiology study), our Child Life specialists will insure that you and your child’s experience is as easy as possible. In February 2012, we opened a new, state-of-the-art Pediatric Endoscopy unit with the newest equipment in a friendly and appropriate space for children, adolescents and their families.
An evaluation may also include radiology studies such as Upper GI series, Magnetic Resonance Enteroscopy (MRE), as well as other imaging techniques when indicated. Our colleagues in Pediatric Radiology use techniques that significantly limit radiation exposure to pediatric patients without compromising the quality of the study.
Our Program’s Philosophy
Each child with IBD is cared for by a primary gastroenterologist and an IBD nurse who are part of a larger team that contributes to your child's care.
You and your family play a key role on “Your IBD team.”
Your IBD team may include nutritionists, pediatric surgeons, social workers, stoma therapists, ophthalmologists, dermatologists, and psychiatrists or psychologists when necessary.
Education about IBD is very important in achieving the best outcomes. All new patients meet along with the family for a private teaching session about IBD. We will offer additional educational experiences on websites we have verified as credible. We encourage you and your child to ask questions and actively participate in all decisions affecting you or your child's care.
Research and new knowledge result in improvements in patient care and we offer our patients the opportunity, if they choose, to be part of studies that will lead to better care of children with IBD. Our IBD program is one of the largest contributors to the Improve Care Now IBD Registry.
Communication and accessibility are important to us. We have a direct phone number that is answered directly by the IBD nurse 1-877-PEDI-IBD (1-877-733-4423) and a page number that is answered 24/7 by a member of the GI staff.
Patient Resources
View the full collection of patient resources from the Pediatric IBD Center.
Parent/Patient Advisory Team
The Parent/Patient Advisory Team (PPAT) is a group of parent and patient volunteers dedicated to working in partnership with the MGfC IBD Center physicians and care team. The mission of PPAT is to help improve care and outcomes for children and adolescents receiving treatment for Inflammatory Bowel Diseases (IBD).
A diagnosis of IBD can be overwhelming and confusing. We understand how this disease impacts patients and families because we live it every day. Our goal is to help empower, support, and educate patients and families along their IBD journey. This is accomplished through ongoing educational programs organized throughout the year. In addition, we are committed to creating a supportive community through social programming and mentoring.
IBD can be a very isolating disease and our philosophy is that no one should worry alone. We are a group who understands the stress, worry, and challenges that IBD can cause, but we also know that patients can thrive and live happy and fulfilling lives. For more information and to join our email list, contact us at: MGHIBDPPATSupport@partners.org.
Conditions and Diseases
Crohn’s disease
Crohn’s disease is diagnosed more frequently in young adults than in children, but children can develop Crohn’s. Crohn’s disease is a form of inflammatory bowel disease (IBD) that can affect different parts of the gastrointestinal tract from the mouth to the anus. The most common part of the digestive tract to become inflamed is the lower part of the small bowel, called the ileum. Other common areas include the esophagus, stomach, duodenum, appendix, and colon.
Crohn’s disease does not have to affect the entire gastrointestinal tract (and rarely does). It can “skip” areas (normal areas between two inflamed areas). The inflammation goes deep into the tissues of the digestive tract and alters the entire thickness of the intestinal walls.
Learn more
Ulcerative Colitis
Ulcerative Colitis is a form of inflammatory bowel disease (IBD) that mostly affects the large intestine (colon). A special feature of ulcerative colitis is that it always starts in the rectum. The inflammation is also continuous, which means there are no skipped areas like there can be in Crohn’s disease. Ulcerative colitis affects only the innermost layer of the bowel wall, called the mucosa, and the inflammation does not penetrate through the other layers (as it does in Crohn’s).
Learn more
Research & Clinical Trials
Our IBD Program also has an active research program in which patients will have the opportunity to participate in research studies trying to understand the relationship between IBD, intestinal bacteria, genetic factors, and the role that certain diets have on IBD. Our center has been selected to participate in many clinical trials of new medications for children who may not have responded to currently approved and available treatments.
Some of our clinical trials include:
- Safety and effectiveness registry for adalimumab (Humira)
- Long-term (20 years) safety registry for infliximab (Remicade)
- Genetics of very early onset IBD
- Role of the genetic markers to determine response to treatment with mesalamine
- Efficacy study of mesalamine (Lialda) for treatment of mild to moderate ulcerative colitis
- Efficacy study of adalimumab (Humira) for treatment of moderate to severe ulcerative colitis
- Role of the microbiome as a biomarker for progression of IBD
- Role of the microbiome in patients with primary sclerosing cholangitis
- Role of the microbiome in children with perianal Crohn’s disease
- Effectiveness of the addition of methotrexate in Crohn’s disease patients starting anti-TNFα therapy
- Infliximab dose escalation in children with Crohn’s disease and ulcerative colitis
Meet the Team
- Harland S. Winter, MD
- Jeffrey A. Biller, MD
- Tracey DaFonte, MD
- Esther Jacobowitz Israel, MD
- Jess Kaplan, MD
- Christopher J. Moran, MD
- Angela Ventura, RN
- Randee Rubenstein, RN
- Camilla Sutter, MA, CCLS (Child Life Specialist)
- Jamie Rossi, MS, CCLS (Child Life Specialist)
International Improvement Learning Network
The IBD Center at MGfC is a member of an international improvement learning network called ImproveCareNow (ICN). ICN connects over 110 other pediatric IBD care centers throughout the world with the goal of improving care for children and adolescents with inflammatory bowel disease.
The ICN network allows patients and families to connect through its publications, parent and patient working groups, and online programs. The ICN website has helpful information and tools for families. You can join the ICN Circle here; please be sure to select “MGfC” as your center.
By signing up you will get:
- A bi-weekly email where you can read stories about how patients, parents, clinicians & researchers are working together to improve care for kids with IBD
- Opportunities to play a direct role in improving care & outcomes by participating in quality improvement projects
- Opportunities to preview new IBD tools & resources, as well as stay up-to-date with research updates
What Is Ulcerative Colitis?
Ulcerative Colitis is a form of inflammatory bowel disease (IBD) that mostly affects the large intestine (colon). A special feature of ulcerative colitis is that it always starts in the rectum. The inflammation is also continuous, which means there are no skipped areas like there can be in Crohn’s disease.
What Are the Symptoms of Ulcerative Colitis?
- diarrhea (sometimes with blood or pus)
- abdominal and/or rectal pain
- rectal bleeding
- urgency to defecate
- weight loss
- fatigue
- fever
What Are the Possible Complications of Ulcerative Colitis?
- Severe bleeding (may lead to iron deficiency anemia)
- A hole in the colon (perforated colon)
- Severe dehydration
- Liver disease (rare)
- Bone loss (osteoporosis)
- Inflammation of your skin, joints and eyes, and sores in the lining of your mouth
- An increased risk of colon cancer
- A rapidly swelling colon (toxic megacolon)
- Increased risk of blood clots in veins and arteries
What Are the Types of Ulcerative Colitis?
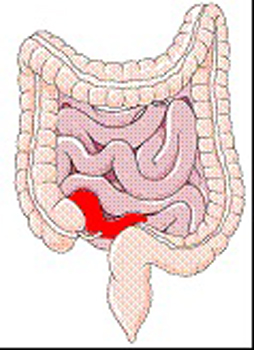
-
Proctitis
This type of ulcerative colitis is when the very end of the large intestine is inflamed.
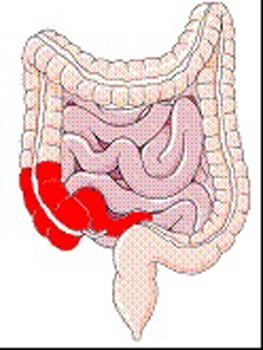
-
Left-Sided Colitis
This type of ulcerative colitis is when one-third of the large intestine is inflamed.
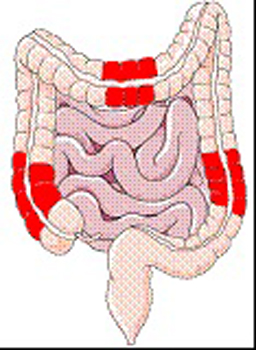
-
Extensive Colitis
This type of ulcerative colitis is when the inflammation stretches over half of the large intestine.
-
Pancolitis
This type of ulcerative colitis is when there is inflammation that involves the entire large intestine.
How Often Should My Child Have a Colonoscopy?
Children with ulcerative colitis (and Crohn’s disease) often will have colonoscopies when their symptoms increase and your doctor is discussing changing the treatment.
In addition, people with colitis (either from ulcerative colitis or Crohn’s disease) have an increased risk of colon cancer over the course of their lifetime. It is recommended to start screening colonoscopies 7 to 8 years after the diagnosis of ulcerative colitis (or Crohn’s disease of the large intestine) and to have them at regular intervals. This test should be done even if your child is feeling well. Factors that increase the risk of colon cancer are a larger area of inflammation, how long the inflammation has been there and some liver problems associated with colitis.
Learn more about ulcerative colitis
What is Crohn's disease?
Crohn’s disease is a form of inflammatory bowel disease (IBD) that can affect different parts of the gastrointestinal tract from the mouth to the anus. Crohn’s disease does not have to include the entire gastrointestinal tract (and rarely does). It can “skip” areas (normal areas between two inflamed areas).
What are common types of Crohn's disease in children?
- Ileitis – Ileitis is when there is Crohn’s disease just in the end of the small intestine.
- Colitis – Colitis is when there is inflammation in just the large intestine. It is the medical word for inflammation in the colon and can either describe Crohn’s colitis (Crohn’s disease of the colon) or ulcerative colitis (another form of IBD).
- Ileocolitis – Ileocolitis is when there is Crohn’s disease in parts of both the large intestine (colon) and small intestine.
Crohn’s disease can also affect the upper part of the gastrointestinal tract such as the stomach or the esophagus (the tube that connects the mouth to the stomach).
What are the symptoms of Crohn’s disease?
Symptoms of active Crohn’s disease include:
- The symptoms of Crohn’s disease vary based on the location and extent of the inflammation in the GI tract. Patients with relatively minor inflammation will experience milder symptoms, while patients with extensive inflammation will have more severe symptoms. Some patients will have flare-ups more frequently than others, who may go into remission for longer periods of time.
- Crohn’s disease can also affect the upper part of the gastrointestinal tract such as the stomach or the esophagus (the tube that connects the throat to the stomach).
- Fevers
- Diarrhea
- Abdominal pain
- Weight loss
- Weakness
- Blood in stools
- Rectal bleeding
- Joint pain
- Skin rashes
What are the complications of Crohn's disease?
Some children with Crohn’s disease have scarring or narrowing in their intestines. This is called a stricture. Strictures can cause abdominal pain and vomiting, and can lead to a blockage in the bowel. Some narrowed areas are caused by inflammation that gets better with medicine. Others can have scar tissue (fibrosis) that may need to be inflated with a balloon during a colonoscopy or, in some children, surgery.
Another possible complication seen in Crohn’s disease is a fistula. A fistula is a connection from one part of the intestine to another part of the body (like another part of intestine, bladder or skin). Fistulae may respond to anti-inflammatory medicines, but some may require surgery.
Sometimes a fistula can lead to a pocket of infection (called an abscess). Abscesses require antibiotics. They may also need to be drained by a radiologist with a tube or by surgery.
Fall 2021 Newsletter: Back to School
Inflammatory Bowel Disease and Coronavirus FAQ
Get answers about coronavirus from the experts at the Pediatric Inflammatory Bowel Disease Center at Mass General for Children.
Appointments and Referrals
Request an appointment or second opinion, refer a patient, find a doctor or view test results with MGfC's secure online services.

