Cutaneous Biology Research Center
Marneros Lab

Contact Information
Cutaneous Biology Research Center
CNY-Building #149
149 13th Street
Charlestown,
MA
02129-2000
Phone: 617-643-7170
Fax: 617-726-2120
Email: amarneros@mgh.harvard.edu
Alexander G. Marneros, MD, PhD
Physician Investigator, Cutaneous Biology Research Center, Massachusetts General Hospital
Associate Professor of Dermatology, Harvard Medical School
Explore This Lab

Overview
Our laboratory is interested in mechanisms that affect wound healing, epithelial biology, inflammation, angiogenesis and fibrosis. Our work has a particular focus on how these processes affect age-related diseases, such as age-related macular degeneration or chronic kidney disease.
News from Our Laboratory
- March 2025: our lab received highly competitive 3-year LEO foundation award: “Aplasia cutis pathogenesis provides key insights into skin and skin appendage biology”.
- February 2024: How a Chance Encounter Led One Mass General Researcher on a Decade-Long Journey of Discovery
For Alexander Marneros, MD, PhD, a dermatologist and researcher at Massachusetts General Hospital, a decade-long journey of discovery began with a chance encounter on his way to lunch. - December 2023: Our paper that identifies the pathomechanisms and cellular origin of aplasia cutis congenita has now been published in the Journal of Clinical Investigation. This work identifies loss-of-function of KCTD1/KCTD15 complexes in cranial neural crest cells as a cause for aplasia cutis.
Mass General Press release - December 2023: Our paper that uncovers a role of AP-2a/AP-2b transcription factors for epidermal homeostasis and skin inflammation has now been published in the Journal of Investigative Dermatology.
- April 2022: Our paper that defines the roles of AP-2a and AP-2b transcription factors for distal nephron development and function has been accepted by Nature Communications.
- November 2021: Our paper that defines key pathways regulating macrophage polarization states and that identified chemical inhibitors of IL-4-induced macrophage polarization has been published in, Cell Reports.
Mass General Press Release - January 2021: Our paper “Magnesium and calcium homeostasis depends on KCTD1 function in the distal nephron” has been published in Cell Reports.
Mass General Press Release - November 2020: Our paper on “Distinct effects of complement and of NLRP3- and non-NLRP3 inflammasomes for choroidal neovascularization” has been accepted by eLife.
Mass General Press Release -
June 2020: Identification of a critical role of AP-2b and KCTD1 for kidney development and renal fibrosis published in Developmental Cell.
We show that the transcription factor AP-2b induces differentiation of distal tubule precursors into early stage distal convoluted tubules (DCTs), whereas its downstream target KCTD1 is required for their terminal differentiation into mature DCTs. KCTD1 loss causes immature DCTs, leading to a salt-losing tubulopathy followed by renal fibrosis via b-catenin hyperactivation.
“AP-2b/KCTD1 Control Distal Nephron Differentiation and Protect against Renal Fibrosis”, Developmental Cell (2020), https://doi.org/10.1016/j.devcel.2020.05.026
- Our Laboratory receives for second time competitive Age-related Macular Degeneration Research Award from the BrightFocus foundation.
- Our laboratory receives two new NIH R01 grants to study novel mechanisms in kidney development and renal fibrosis.
- Our lab receives two new R01 grants from the NIH/NEI to investigate the role of macrophages and inflammasomes in neovascular age-related macular degeneration.
Research Projects
Research Program I: From wound healing to the identification of novel regulators of epithelial differentiation and fibrosis.
We use human genetics to identify critical regulators of skin formation and wound healing by discovering the gene mutations that cause aplasia cutis congenita (ACC), which manifests with scalp skin defects at birth. Originating from a chance encounter with a family with ACC, we identified the first gene for ACC as the ribosomal GTPase BMS1 that, when mutated, leads to a ribosome biogenesis defect and a ribosomal stress response (PLoS Genetics, 2013). We also discovered causative gene mutations in KCTD1 in patients with Scalp-Ear-Nipple (SEN) syndrome who have ACC and additional abnormalities (Am J Hum Genet, 2013). We generated mice that lack KCTD1 and found, unexpectedly, that KCTD1 is a critical regulator of distal nephron differentiation: KCTD1 deficiency leads to a terminal differentiation defect in the distal nephron that causes a salt-losing tubulopathy and progressive renal fibrosis. Based on the findings in Kctd1mutant mice, we reassessed SEN syndrome patients with KCTD1 mutations and found that they also develop progressive renal fibrosis, linking a critical role of KCTD1 in epithelial differentiation processes in both the skin and the kidney. Our detailed mouse genetics approaches showed that an AP-2b/KCTD1 axis controls the development of distal convoluted tubules and is also required for the maintenance of their terminal differentiation state in the adult. Loss of terminal differentiation of the distal nephron owing to lack of AP-2b or KCTD1 leads to progressive renal fibrosis due to b-catenin hyperactivation and increased mTOR activity (Dev Cell, 2020). Moreover, we found that KCTD1 is a key regulator of magnesium and calcium transport processes in the distal nephron (Cell Reports, 2021). These findings represent a major contribution to our understanding of the mechanisms that orchestrate distal nephron differentiation and have important translational relevance for SEN syndrome patients, who may benefit from mTOR inhibitors. We also found that the two related transcription factors AP-2a and AP-2b have distinct spatiotemporal roles in separate segments of the distal nephron, where they regulate their function (Nature Communications, 2022). The findings in the kidney guided us to uncover key roles of AP-2a/AP-2b and KCTD1 also for skin appendage formation and we were now able to identify the cellular origin and pathomechanisms of ACC, answering the centuries-old enigma of why ACC mainly affects the scalp skin (J Clin Invest, 2023; J Invest Dermatol, 2024). Thus, this research program connects my clinical encounters to my interdisciplinary laboratory investigations that discovered fundamental mechanisms in epithelial differentiation programs, which are in part shared in the skin and the kidney. Our discoveries provide the framework for novel therapies.
.
Research Program II: From wound healing to macrophage polarization mechanisms and angiogenesis.
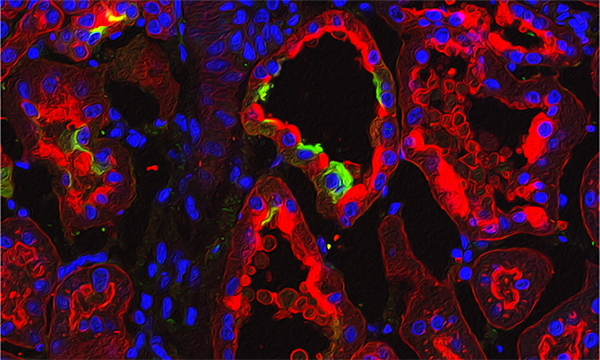
Aberrant angiogenesis exacerbates wound healing disorders, neovascular age-related macular degeneration (AMD), or tumor growth. We found in animal models of wound healing and neovascular AMD that polarization of macrophages to a proangiogenic subtype strongly promotes inflammatory angiogenesis, which can be blocked by ablation of these macrophages (Cell Reports, 2013; Am J Pathol, 2013; J Biol Chem, 2014). Identifying drugs that prevent this polarization process represents an important unmet clinical need. Global quantitative time-course proteomics, phosphoproteomics, and transcriptomics allowed us now to identify specific signaling nodes that are required for macrophage polarization processes. Drug screens identified drugs that selectively inhibited IL-4-induced proangiogenic macrophage polarization by blocking some of these signaling nodes. For example, we found that a MEK/PPARg/retinoic acid signaling axis is required for IL-4-induced macrophage polarization. We validated the clinical significance of these findings in mouse models of wound healing and neovascular AMD (Cell Reports, 2021). Our recent results offer exciting novel therapeutic opportunities to improve various diseases that are promoted by these polarized proangiogenic macrophages
Research Program III: From wound healing to inflammasomes and neovascular AMD.
We investigate pathomechanisms that drive neovascular AMD, as this disease is promoted by inflammation that resembles a prolonged wound healing reaction. Progress in this field has been limited by a lack of a mouse model that forms spontaneous choroidal neovascularization (CNV). We identified a genetic mouse model for neovascular AMD that develops spontaneous CNV and AMD pathologies similarly as observed in the human disease, Vegfahyper mice. CNV forms in these mice as a consequence of chronically increased VEGF-A in the retinal pigment epithelium (RPE) (Cell Reports, 2013, FASEB J, 2014). This AMD mouse model confirmed the critical role of pro-angiogenic macrophages for CNV formation. Moreover, we discovered that increased NLRP3 inflammasome activation promotes CNV via secretion of proangiogenic IL-1b, whereas genetic or pharmacologic targeting of inflammasomes potently inhibits CNV (EMBO Mol Med, 2016). Our recent new data answer key unresolved questions in the AMD field and show that not only NLRP3-dependent but also NLRP3-independent inflammasome activation in macrophages and microglia, but not in RPE cells, promotes CNV (eLife, 2020). These findings have important clinical relevance and suggest that inflammasome inhibitors can improve current neovascular AMD therapies.
Research Positions
A Postdoctoral Research Fellow position is available for a highly qualified individual with expertise in biochemical assays and mouse in vivo work. Experience in computational biology is preferred. Interested candidates should send their information including CV and the name of 2-3 references to Dr. Alexander G. Marneros: amarneros@mgh.harvard.edu
Lab Members
CURRENT LAB MEMBERS
Ivy Zhong
Jackelyn Raymundo
Bill Senapati
Arjun Ahilan
Christina Eng
Publications
Selected Publications
Raymundo J, Makkar J, Fasci M, Driskell R, Marneros AG. TGFa is required for hair follicle function during aging and its loss leads to progressive alopecia. J Invest Dermatol., 2025, in press.
Zhang H, Raymundo J, Daly KE, Zhu, W, Senapati B, Zhong H, Ahilan AR, Marneros AG. AP-2a/AP2b transcription factors are key regulators of epidermal homeostasis. J Invest Dermatol., 2024; doi: 10.1016/j.jid.2023.12.017.
Senapati B, Raymundo J, Makkar J, Driskell R, Marneros AG. KCTD1/KCTD15-Mediated Repression of AP2α/AP-2β is Required for Proper Skin Appendage Development and Epidermal Homeostasis. J Invest Dermatol., 2025, S0022-202X(25)02832-5.
Raymundo J, Zhang H, Smaldone G, Zhu W, Daly, KE, Glennon BJ, Pecoraro G, Salvatore M, Devine WA, Lo C, Vitagliano L, Marneros AG. KCTD1/KCTD15 complexes control ectodermal and neural crest cell functions and their impairment causes aplasia cutis. J Clin Invest., 2023; e174138. doi: 10.1172/JCI174138.
Lamontagne JO, Zhang H, Zeid AM, Strittmatter K, Rocha AS, Williams T, Zhang S, Marneros AG. Transcription factors AP-2a and AP-2b regulate distinct segments of the distal nephron in the mammalian kidney. Nature Communications, 2022; 13(1): 2226. doi:10.1038/s41467-022-29644-3.
Zeid AM, Lamontagne JO, Zhang H, Marneros AG. Epidermal growth factor deficiency predisposes to renal disease. FASEB J, 2022; e22286; doi:10.1096/fj.202101837R.
He L, Jhong JH, Chen Q, Huang KY, Strittmatter K, Kreuzer J, DeRan M, Wu X, Lee T, Slavov N, Haas W, Marneros AG. Global characterization of macrophage polarization mechanisms and identification of M2-type polarization inhibitors. Cell Reports, 2021, 37(5), 109955.
Marneros AG. Magnesium and calcium homeostasis depends on KCTD1 function in the distal nephron. Cell Reports, 2021; 34(2): 108616. doi: 10.1016/j.celrep.2020.108616
Malsy J, Alvarado AC, Lamontagne JO, Strittmatter K, Marneros AG. Distinct effects of complement and of NLRP3- and non-NLRP3 inflammasomes for choroidal neovascularization. eLife, 2020, e60194.
Marneros AG. AP-2b/KCTD1 Control Distal Nephron Differentiation and Protect against Renal Fibrosis, Developmental Cell. 2020, https://doi.org/10.1016/j.devcel.2020.05.026
Marneros AG. Effects of chronically increased VEGF-A on the aging heart. Am J Pathol. 2018 Mar;32(3):1550-1565. doi: 10.1096/fj.201700761RR.
Strittmatter K, Pomeroy H, Marneros AG. Targeting PDGFRβ+ scaffold formation inhibits choroidal neovascularization. Am J Pathol. 2016, 186(7):1890-9.
Marneros AG. Increased VEGF-A promotes multiple distinct aging diseases of the eye through shared pathomechanisms. EMBO Mol Med. 2016, 8(3): 208-231. PMID: 26912740.
Marneros, AG. Genetics of aplasia cutis reveal novel regulators of skin morphogenesis. J Invest Dermatol. 2015, 135(3):666-672. PMID: 25355129.
Ablonczy Z, Dahrouj M, Marneros AG.Progressive dysfunction of the retinal pigment epithelium and retina due to increased VEGF-A levels. FASEB J. 2014, May;28(5):2369-79. doi: 10.1096/fj.13-248021.
He L, Marneros AG. Doxycycline inhibits polarization of macrophages to the proangiogenic M2-type and subsequent neovascularization. J Biol Chem. 2014, Mar 21;289(12):8019-28. doi: 10.1074/jbc.M113.535765.
He L, Marioutina M, Dunaieff J, Marneros AG. Age- and gene dosage-dependent Cre-mediated abnormalities in the retinal pigment epithelium. Am J Pathol. 2014, Jun;184(6):1660-7. doi: 10.1016/j.ajpath.2014.02.007.
Marneros AG. NLRP3 Inflammasome Blockade Inhibits VEGF-A-Induced Age-Related Macular Degeneration. Cell Reports. 2013, 4(5): 945-958. Cover article.
He L, Marneros AG. Macrophages are essential for the early wound healing response and the formation of a fibrovascular scar. Am J.Pathol. 2013 182(6):2407-17 Cover article.
Marneros AG. BMS1 is mutated in Aplasia Cutis Congenita. Plos Genetics. 2013, 9(6):e1003573.
Marneros AG, Beck AE, Turner EH, McMillin MJ, Edwards MJ, Field M, de Macena Sobreira NL, Perez AB, Fortes JA, Lampe AK, Giovannucci Uzielli ML, Gordon CT, Plessis G, Le Merrer M, Amiel J, Reichenberger E, Shively KM, Cerrato F, Labow BI, Tabor HK, Smith JD, Shendure J, Nickerson DA, Bamshad MJ; University of Washington Center for Mendelian Genomics. Mutations in KCTD1 cause scalp-ear-nipple syndrome. Am J Hum Genet. 2013 Apr 4;92 (4):621-6.
Makinodan E, Marneros AG. Protein kinase A activation inhibits oncogenic Sonic hedgehog signalling and suppresses basal cell carcinoma of the skin. Exp Dermatol. 2012;21(11):847-52.
Marneros, AG, Blanco F, Husain S, Silvers DN, Grossman ME. Classification of cutaneous intravascular breast cancer metastases based on immunolabeling of blood and lymph vessels. J Am Acad Derm. 2009;60(4):633-8.
Marneros AG, Grossman ME, Silvers DN, Husain S, Nuovo GJ, MacGregor-Cortelli B, Neylon E, Patterson M, O'Connor OA, Zain JM. Pralatrexate-induced tumor cell apoptosis in the epidermis of a patient with HTLV-1 adult T-cell lymphoma/leukemia causing skin erosions. Blood. 2009;113(25):6338-41.
Marneros AG, She H, Zambarakji H, Hashimoto H, Connolly E, Kim I, Gragoudas E, Miller JW, Olsen BR. Endogenous endostatin inhibits choroidal neovascularization. FASEB J. 2007, 21(14):3809-3818.
Marneros AG, Fan J, Yokoyama Y, Gerber HP, Ferrara N, Crouch, RK, Olsen BR. VEGF expression in the retinal pigment epithelium is essential for choriocapillaris development and visual function. Am J Pathol. 2005;167: 1349-1357.
Marneros AG, Keene DR, Hansen U, Fukai N, Moulton K, Goletz PL, Moiseyev G, Pawlyk BS, Halfter W, Dong S, Shibata M, Li T, Crouch RK, Bruckner P, Olsen BR. Collagen XVIII and endostatin are essential for vision and retinal pigment epithelial function. EMBO J. 2004;23(1):89-99.
