Center for Neurointestinal Health
The Center for Neurointestinal Health at Massachusetts General Hospital combines robust scientific investigation with advanced diagnostic and therapeutic care.
The Center for Neurointestinal Health at Massachusetts General Hospital seeks to improve our understanding of and treatment for neurointestinal disorders by providing a continuum between basic research, translational research and clinical care.
We are the only center that provides comprehensive pediatric and adult care coupled with basic and translational research.
Our research program includes:
- A basic research laboratory focused on the enteric nervous system that is funded by the National Institutes of Health (NIH)
- Clinical research studies in pediatric and adult GI motility supported by the NIH, foundations and industry
- Many successful national and international collaborations studying a range of topics related to neurointestinal diseases. These topics include genetics, developmental biology, stem cell therapy, brain-gut connections, novel modes of imaging, and gut motility to name only a few.
Current studies
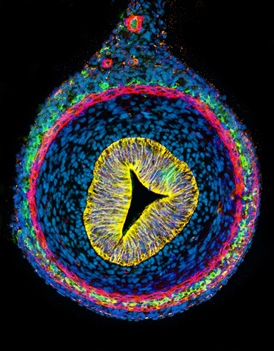
Replacing Nerve Cells in Hirschsprung Disease
Hirschsprung disease, a condition in which nerve cells are absent from the large intestine, affects one in 5,000 children. We have developed methods to isolate stem cells from the intestine and to coax them into becoming nerve cells in a petri dish. We are currently transplanting these new neurons into the colon to replace the missing nerve cells in Hirschsprung disease or to replace abnormal nerves in other neurointestinal diseases. This research offers hope for a novel approach to treat diseases of the intestinal nervous system.
Regulating the Growth Nerve Cells in Inflammatory Diseases
Inflammatory diseases of the intestine, such as Crohn’s disease and ulcerative colitis, can be debilitating conditions leading to severe intestinal inflammation, pain and poor nutrition. We recently discovered that inflammation stimulate the birth of new neurons in the colon. Why this happens, what signals are required, and where those new nerves come from are all unanswered questions. Our current studies are working to discover the mechanisms that promote this process. Identifying the signals that lead to the creation of new neurons in the intestine will allow us to develop novel therapies that harness this remarkable regenerative capacity.
Cell Examination Without Biopsy
Currently, a biopsy is needed to examine nerve cells in the intestine so that a pathologist can look at the nerves under a microscope. This is the standard way of diagnosing Hirschsprung disease. Working with experts in state-of-the-art imaging at Mass General, we are developing a new method that allows clinicians to see nerve cells through the wall of the intestine, during surgery or colonoscopy, without the need to remove any tissue.
Understanding Nerve Communication

The nerves of the intestine control all aspects of gut function, acting in effect as the intestine’s brain. Among their roles, these nerves communicate with the inside lining of the gut to sense the presence of bacteria, food, toxins and waste in the gut lumen.
Little is known about how these nerves sense the intestine’s contents, how they distinguish nutrients from poisons, or how they differentiate healthy bacteria from infectious pathogens.
Our researchers are working to understand how the nerves mediate these critical processes. The results of these studies will impact diverse areas of research related to nutrition, infection and inflammation.
Artificial Intestine
Children and adults with severe intestinal disorders often rely on intravenous nutrition because their intestines cannot maintain their nutritional needs. This condition is called “short bowel syndrome.” While intestinal transplantation is an option, this is a major procedure with significant complications and poor long-term results. In collaboration with other scientists at Mass General Hospital who are experts in organ engineering, we are conducting experiments to create artificial intestines using a patients’ own cells. Successful development of this new technology will hopefully one day eliminate the need for intestinal transplantation.
Understanding the Brain-Gut Connection
Many patients suffer from common gut symptoms such as abdominal pain, hunger and nausea. The brain and the gut are intimately intertwined with information flowing back and forth affecting the function of both resulting in an expression of how we feel and perceive symptoms. Functional brain imaging with MRI is being used in healthy volunteer and patients with various GI conditions to understand the wiring of the brain with these gut sensations, what is abnormal and how therapies might affect the system.
How Does the Gut Move Things from One End to the Other?
Gut motility is such a basic function that we take for granted unless it failed to work. If the gut is slow in the esophagus, stomach, small intestines or colon, pain, nausea, vomiting, constipation and bloating can occur. If severe, malnutrition can occur because of inability to eat or pass what is consumed by mouth. The gut nerve and muscle function drive this process and can malfunction in many different diseases. Our research group has been at the forefront of understand how the gut works to move what is consumed from the mouth to the end. We have helped developed the technology Smartpill Wireless Motility Capsule to help gain insights in health and conditions such as gastroparesis and constipation.
Understanding the Origins of Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome is the prototype for a biopsychosocial illness—that is an illness that reflects a person’s psychosocial environment in addition to biologic changes occurring in the gut. Our group, in conjunction with the Clinical and Translational Epidemiology Unit, is looking at non-traditional, childhood risk factors for the development of IBS in adulthood. We are specifically interested in childhood dietary influences and the role of eating preferences and self-image during adolescence and how these factors influence the likelihood of developing IBS later on.
Unlocking the Mysteries of Chronic Constipation
Constipation is an incredibly common condition affecting much of the population, yet the understanding of its physiologic underpinnings is still primitive. Our research group uses the latest technology to make the connection between a patient’s symptoms and their gut function to determine which treatments may improve symptoms beyond traditional laxative therapies that are currently on offer for different subgroups of patients with constipation. We are also interested in determining the benefits of a holistic approach to constipation that incorporates physical therapy, psychological therapies, and dietary modification in addition to traditional medications in the treatment of chronic constipation.
Examining the Role of Genetics and the Microbiome in Patients with Functional Gastrointestinal Diseases
Our research group is assembling a biobank (repository) of blood and stool specimens from patients with functional GI disease and motility disorders in conjunction with surveys measuring patient-reported outcomes (symptoms) so that we can determine genetic and gut bacterial influences on the presentation of these diseases and their response to treatment. The goal is to use advanced analysis techniques to work toward true personalized medicine for the treatment of patients suffering from functional GI diseases.
Investigating the Distinctions in the Pediatric Patient
Pediatric patients offer a unique presentation of neurointestinal symptoms with underlying etiologies that differ from adults. By studying the distinct traits of pediatric patients we have gained deeper insight into GI motility and functional disorders, thus allowing us to tailor treatment for each individual child.
Through validated therapy and novel approaches, we are focused on understanding the correlation between pediatric symptom characteristics and intervention outcome, hoping to optimize pediatric management. We are currently investigating various treatment options in a wide variety of diseases such as constipation and irritable bowel syndrome both with medication and alternative approaches including physiotherapy, botulinum injections, and psychotherapeutic interventions through our multidisciplinary center.
Support Research at Mass General
Your gift helps fund groundbreaking research aimed at understanding, treating and preventing human disease.
Center for Neurointestinal Health
The Center for Neurointestinal Health at Massachusetts General Hospital combines robust scientific investigation with advanced diagnostic and therapeutic care.
