Overview
Addressing an Unmet Need
Individuals with schizophrenia and bipolar disorder die nearly 30 years earlier than the general population, and cancer is the 2nd leading cause of death among this group. People with serious mental illness are more than twice as likely to die from cancer, less likely to receive timely, high quality cancer care, and more likely to be excluded from clinical trials. Access to early, integrated psychiatric care may improve cancer treatment for patients with mental illness.
Our Mission
Directed by Kelly E. Irwin, MD, MPH, the mission of the Collaborative Care and Community Engagement Program is to promote access to cancer care for every patient who needs us, and to support their families and caregivers. Through clinical innovation, research, education, and advocacy, the Program aims to prevent premature cancer mortality and improve the quality of life of individuals affected by mental illness and cancer.
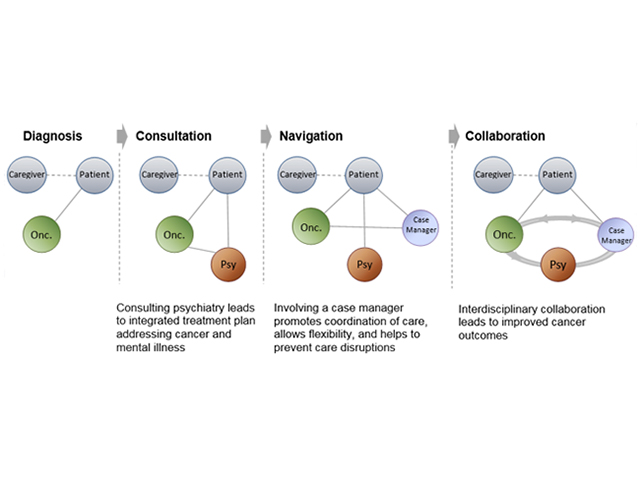
A New Care Model for Patients with Cancer and Severe Mental Illness
In 2016, the Collaborative Care and Community Engagement Program conducted the first-of-its-kind pilot study of a person-centered, team-based approach to cancer care for patients with schizophrenia and cancer. The approach was informed by the collaborative care model and personalized to address the specific challenge of cancer and mental illness:
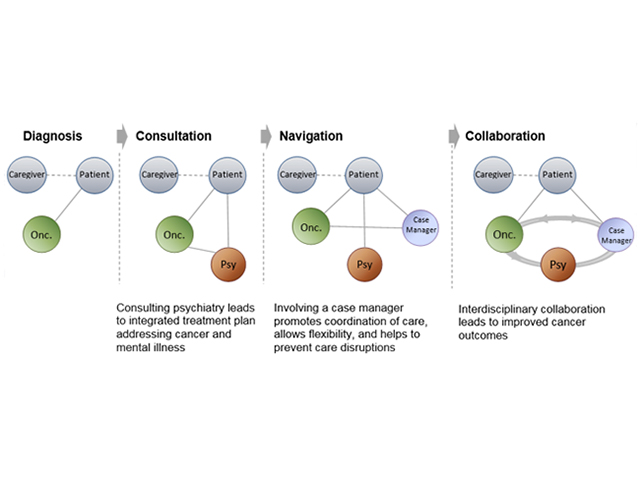
- Person-centered care: Identifying goals and providing continuity across settings
- Screening: Identifying patients at cancer diagnosis, maintaining population-based registry
- Co-management: Partnering with the oncologist to adapt the cancer treatment plan
- Interdisciplinary team: Psychiatry, Oncology, Social Work, Community-Based Clinicians
- Collaboration across systems: Bridging oncology and community mental health
A team-based approach to care, timely access to mental health services, and strong communication with patients and caregivers are essential to helping these men and women get the treatment that they need and deserve.
Dissemination Strategies
View our Dissemination Strategies document.
Stakeholder Needs Assessment
View the needs assessment of our stakeholder groups.
Research
Clinical Trials:
BRIDGE: Proactive Psychiatry Consultation and Case Management for Patients With Cancer
Publications:
Unlearning Our Helplessness — Coexisting Serious Mental and Medical Illness
N Engl J Med. 2016 Oct 27;375(17):1690-1694.
A 63-Year-Old Woman with Bipolar Disorder, Cancer, and Worsening Depression
N Engl J Med. 2016 Sep 29;375(13):1270-81. doi: 10.1056/NEJMcpc1609309.