Integrated Substance Use Disorder Training Program

Contact Information
Integrated Substance Use Disorder Fellowship
55 Fruit Street
Boston,
MA
02114
Samreen Sethi
Program Coordinator
sssethi@mgh.harvard.edu
Martha T. Kane, PhD
Fellowship Director
Clinical Director, Program in Substance Use & Addiction Services (PSAS)
Unit Chief, Behavioral Health, MGH Charlestown Health Center
Massachusetts General Hospital
Kane.martha@mgh.harvard.edu
Program in Substance Use & Addiction Services (PSAS)
This fellowship is part of the Mass General Program in Substance Use & Addiction Services (PSAS). For more information, please visit the PSAS website.
Explore This Training Program
Overview
Twenty-three million Americans have a substance use disorder (SUD), yet only 10% receive treatment annually. Among hospitalized patients, 22% have an active drug or alcohol use disorder. Despite the growing prevalence of SUDs, few clinical providers have the opportunity to gain specialty training in addiction medicine.
The Massachusetts General Hospital Integrated Substance Use Disorder Training Program will prepare nurse practitioners, psychologists and social workers for clinical and academic careers in addiction medicine with a particular focus on developing and enhancing evidence-based addiction prevention and treatment services for all patients, including those vulnerable to health disparities because of poverty, race, culture, age, gender, disability or stigma.
Through a combination of inpatient and outpatient care spanning diverse settings, trainees will receive training in the knowledge and skills to become expert clinicians and leaders in the field of addiction medicine. Clinical rotations include:
- Outpatient addiction treatment provided as a multidisciplinary behavioral health team integrated into primary care at Mass General community health centers
- Low threshold, urgent and transitional addiction treatment in the Mass General outpatient Bridge Clinic
- Dual-diagnosis treatment in Mass General’s specialty outpatient clinics for both adults and youth
- Inpatient consultation on the Addiction Consult Team at serving the entire Mass General Hospital
Electives and longitudinal experiences will be further tailored to each trainee’s interests and guided by the interdisciplinary program faculty. The diverse program faculty includes the following:
- Physicians from Internal Medicine, Psychiatry and Family Medicine
- Psychologists
- Nurse Practitioners
- Recovery Coaches
- Clinical Social Workers
The primary goal of the one-year, full-time training program is to prepare nurse practitioners, social workers and psychologists for clinical and academic careers in addiction medicine. Trainees will benefit from working within the Program in Substance Use & Addiction Services (PSAS), a hospital-/community-wide collaboration to deliver state-of-the-art addiction medicine care for those suffering with substance use issues. This program also benefits from close collaboration with Mass General’s addiction medicine and psychiatry fellowships for physicians and trainees will work together in many shared settings.
Fellows receive benefits through Mass General. More information on benefits can be found on the Mass General website.

Curriculum
Training Experience
Core training includes an overview of the field of addiction medicine with an emphasis on training addiction medicine nurse practitioners, psychologists and social workers who will educate other clinicians and trainees in the community; rigorously assess and incorporate scientific evidence into their practice and deliver compassionate care to a diverse population of patients, particularly those who are most marginalized. Training will comprise didactic and clinical experiences across the spectrum of addiction care, including the following:
- Comprehensive behavioral treatment of the full spectrum of substance use disorders using evidence-based models
- Psychosocial interventions to address social determinants of health in substance using populations
- Harm reduction
- Motivational interviewing
- Focus on providing care for vulnerable populations
- Neurobiology of addiction
- Pharmacotherapy for substance use disorders
- Novel and integrated care models for substance use disorder treatment
Core Clinical Sites
- Massachusetts General Hospital
- Mass General Community Health Centers
Clinical Experience Area
- Outpatient Addiction Treatment within a Community Health Center: 12-month longitudinal rotation within an integrated care setting at a Mass General primary care health center
- Inpatient Consultation Service at Mass General: Rotation on the Mass General inpatient Addiction Consultation service. The multidisciplinary Addiction Consult Team (ACT) offers expert consultation and support for patients with moderate to severe substance use disorders (SUDs) across Mass General’s inpatient units
- Outpatient Co-occurring Disorders Rotation: Outpatient rotation providing treatment for co-occurring disorders at the Mass General Addiction Recovery Management Services (ARMS) and West End Clinic
- Mass General Bridge Clinic: Rotation in a low barrier, transitional outpatient addiction clinic for vulnerable patients who are unable to benefit from more traditional outpatient SUD care. Patients served include discharged inpatients with unstable outpatient options, patients leaving the emergency department who are not yet connected to outpatient care, and primary care patients who are not stable enough to benefit from structured care. The Bridge Clinic provides patients with continued necessary treatment for their SUDs delivered in a patient centered, patient determined approach until they stabilize enough that they can access appropriate community-based treatment.
- Mass General HOPE Clinic: Rotation in a perinatal clinic for families impacted by substance use disorder. The HOPE Clinic is interdisciplinary, offering obstetrics, pediatric, family medicine, addiction and psychiatric care for the birthing person, partner and child(ren) from pregnancy through the first two years of the child’s life.
Elective Rotation
Trainees will have 24 weeks of an elective rotation. Electives will offer fellows an opportunity to deepen their experience in one of the areas of required training, including Inpatient care, Low Threshold Care, Integrated Primary Care, care for co-occurring disorders, and care for pregnant and post-partum families. Trainees may also create custom electives with the help of the program director focused on their unique interests.
Trainees learn to work in a team-based model with other professionals, including counselors, social workers, nurses, psychologists, recovery coaches and physicians from a variety of specialties. Teams will be based in outpatient treatment agencies, outpatient primary care settings and within community-based teams providing essential services to those suffering with substance use disorder.
Academic Preparation
Trainees will have weekly didactic sessions delivered by experts in a broad range of topics related to providing care for those with substance use disorder. Trainees will have the opportunity to participate with addiction medicine fellows and addiction psychiatry fellows in applicable didactic opportunities. In addition, fellows will have the opportunity to become involved in ongoing research projects as one of their elective rotations as time and interest allow.
Mentorship and Career Development
Mentorship and career development is an important aspect of our program. Within the first three months of the program, each fellow has the opportunity to meet with our Program Director and faculty to discuss career goals. The Program Director and faculty concretely explore fellows’ career aspirations including geography and type of position and provide guidance on the job search process, including where to search for posted job opportunities and what networking opportunities exist at local and national meetings. The program director and faculty directly connect fellows to relevant colleagues based on fellows’ interests and utilize their own professional networks to make introductions for fellows to speak with leaders in the field in geographic regions of interest to begin exploring job opportunities. In addition, our faculty represent a variety of diverse care settings and are eager to support and mentor fellows depending on their interests. After the initial meeting, career planning sessions continue monthly for the remainder of the training year.
United Against Racism
As a key training program in the Mass General Program in Substance Use & Addiction Services (PSAS), the ISTP fellows will be able to be involved in the ongoing United Against Racism initiative. Launched in the Fall of 2020, United Against Racism exemplifies the power of systemwide collaboration and is an important part of how we are transforming Mass General Brigham to become the integrated academic healthcare system of the future, with patients at the center. Individuals and teams across every member organization, department, and job function play an instrumental role in advancing this work.
Our Team
Current Fellows
Integrated Substance Use Disorder Training Program Fellows 2025-2026
 James M. Edgerton, LCSW (he/him)
James M. Edgerton, LCSW (he/him)
Preferred name: Mac
Mac is a licensed clinical social worker who completed his undergraduate education at the University of Vermont and received his Master of Social Work from Boston College School of Social Work. With experience in outpatient and community settings throughout the Boston area, he remains committed to deepening his knowledge and impact in the treatment of adult mental health and substance use disorders. Prior to entering the field of social work, Mac worked in the documentary film industry in New York City, where he developed a deep appreciation for storytelling, empathy, and the power of human connection – values that continue to shape his clinical practice today. Mac intends to continue his clinical work with a focus on delivering compassionate, evidence-based care for substance use and mental health disorders through a harm reduction lens.
 Sandya Janardhan, PMHNP-BC (she/her)
Sandya Janardhan, PMHNP-BC (she/her)
Sandya Janardhan is a board-certified Psychiatric-Mental Health Nurse Practitioner (PMHNP-BC) from the University of Pennsylvania with a strong commitment to providing care to individuals with complex trauma, serious mental illness, and underserved mental health needs. A top graduate of her program, she was awarded a full scholarship as a Lauder Fellow—an accolade granted to only ten students. Following graduate school, Sandya worked in Chicago, Illinois, as a psychiatric nurse practitioner, providing substance use care in an outpatient, community-based setting. Prior to her advanced practice training, she brings extensive experience as a critical care registered nurse in the Detroit and Ann Arbor, Michigan areas.
 Natacha Nortelus, FNP, PMHNP-BC (she/her)
Natacha Nortelus, FNP, PMHNP-BC (she/her)
My name is Natacha Nortelus, I am a dual board-certified Nurse Practitioner (FNP and PMHNP-BC). I grew up in Haiti and moved to the United States 24 years ago. I earned both my bachelor’s and master’s degrees in nursing from the University of Massachusetts Boston and worked in various roles and settings at Massachusetts General Hospital for 16 years.
Early in my career as a registered nurse, I discovered a deep sense of fulfillment in caring for individuals with substance use disorders. However, despite my passion, I often felt limited in the care I could provide due to a lack of specialized training. In 2024, I earned a doctorate degree from the University of Alabama and a post-master’s certificate in psychiatry from Wilkes University, fulfilling my longtime dream of acquiring the training that will allow me to provide that compassionate, patient-centered care to individuals with substance use disorders.
In my free time, I enjoy reading and watching historical novels and shows. I also love traveling and hope to visit many of the places I have explored through my books.
Learn more about our past fellows

How to Apply
Eligibility
Eligible candidates will be from one of the below disciplines and meet the following criteria:
- Nurse Practitioners: Master of Science in Nursing (MSN). Current licensure as a Nurse Practitioner or Clinical Nurse Specialist in the Commonwealth of Massachusetts. Mass Controlled Substances Licensing
- Psychologists: PhD, PsyD or EDD in Psychology
- Social workers: Master of Social Work (MSW) degree required. Massachusetts license (LICSW or LCSW)
All applicants should have an interest in providing substance use disorder care in under-resourced, community-based settings.
Timeline & Process
If you have any questions, please contact:
Samreen Sethi
Program Coordinator
sssethi@mgh.harvard.edu

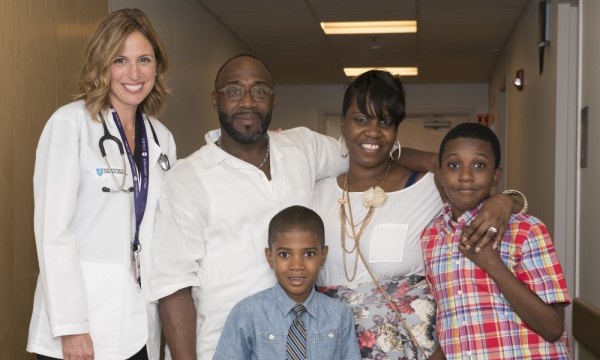
A patient (and his partner) who received care at the West End Clinic, one of the sites for the Integrated Substance Use Disorder Training Program.

Dawn Williamson, a nurse practitioner on the Addiction Consult Team, in the Emergency Department.
