Postpartum Traumatic Stress Disorders Research Program


Contact Information
For questions regarding study participation, please e-mail our team at MothersStudy@partners.org
Explore This Research Lab
Overview
Ensuring the well-being of women from the very early postpartum period is important for mother and child health. Research in the Dekel lab at Massachusetts General Hospital is focused on identifying the factors that are implicated in optimal adaptation as well as psychopathology of mothers following childbirth. To this end, we combine psychological, physiological and neuroimaging tools to prospectively study women from pregnancy across childbirth. Ultimately our goal is to develop novel tools for early detection of mothers at risk for postpartum mental disorders and preventive treatments that are effective and safe.
Although childbirth is usually considered a uniformly happy event, some women may experience a traumatic childbirth. Some will go on to develop a postpartum posttraumatic stress disorder (PTSD), a condition we know very little about. We study the psychological and biological mechanisms underlying the various mental health trajectories in the wake of a traumatic delivery and what allows some women to be resilient and even grow psychologically. We are also interested in learning the ways in which distress in the mother may influence child development.
Patient Stories
There’s a recurrent theme among birthing people who experience a traumatic birth, only 20% seek treatment because there’s no formal diagnosis for postpartum PTSD. Women too often don’t know they’re suffering with the condition and can experience guilt and shame.
Increasing awareness of conditions of traumatic stress and associated post-traumatic stress disorder (PTSD), which is different and distinct from postpartum depression (PPD), after giving birth can help destigmatize postpartum PTSD, promote healing and a sense of ‘you’re not alone.’
Please be advised that the stories below are honest and powerful, though traumatic, stories of childbirth.
Emergency and/or unscheduled cesarean section (c-section)
“It’s after 6am and I wake up in my bed at the delivery room to see a group of nurses standing at my bedside looking very concerned. I immediately can tell that something’s not right. One of the nurses tells me that my baby’s heart rate has spiked really high and isn’t coming down. I start to panic and feel my heart beat faster and my stomach in knots. Two or three minutes later the nurses rush back in and one of them tells me that I need a c-section right now. I ask whether my partner can come and the nurse tells me they have to take me immediately. She puts a hairnet on me as they’re rushing me down the hall. I feel like I have no control. I hold on to my necklace with my daughter’s ashes and pray. I’m all alone and I’m terrified that I’ll lose this baby too.”
Recovery/immediate postpartum
“It’s the morning and I'm in the bathroom. I’ve just urinated. Now, I feel something large slide out of me as I stand up. Looking down, my face becomes flushed. There, on the pad in my underwear, I see a very large blood clot approximately the size of a lime. I’m feeling nauseous and my heart quickens. I fear that I’m bleeding again. With my hands trembling, I pull the nurses’ emergency line. Then, 3 nurses come running into the bathroom, and I see they look panicked. I feel lightheaded and jittery. I’m scared I need another surgery.”
Health of the fetus
“It’s around 11 am and I’m lying on a bed in the operating room and I’ve just had a c-section. They drop the curtain to show me my baby, and I feel sweaty as I look at her. She looks very red and swollen, and I know that something is wrong. My husband tells me that she has swelling on her head because she couldn’t fit, and I feel guilty because she was trying, and I wasn’t helping her. I feel exhausted as I think about what’s going to happen next. With tension in my forehead, I hear the constant chatter between the doctors, but no one will tell me if I’ll be able to do skin to skin and I feel sad.”
Obstetrical complications
“I’m lying cut open on the operating room table and blood rushes to my head. I don’t hear my baby crying, and I think that she’s not alive. They take my baby away, and I see my husband walk past me, looking at me with my insides exposed. The surgeon says, “I don’t like the placement of the bowel, let’s take it out and place it again.” I break out into a sweat and start to have a panic attack as my heart beats faster. Then, I begin to black out and my hands start to shake as I become nauseous.”
Medical complications
“It’s 11:00 pm and I’m lying on the operating room table with three IVs restricting my arms. My husband isn’t in the room and I’m all alone. Bright light shines on me, and my eyes become watery. Immediately I feel sick and begin to vomit. The nurse gives me a puke bag and I’m barely holding it between my left shoulder and chin. Only some of the vomit makes it in. I continue to shake vigorously and feel no control over what is happening. Now, the doctor tells me she needs to do a hysterectomy. My body feels heavy as I think I’ll lose my uterus. I’m concerned I may even lose my life.”
Staff interactions
“It’s around 9:30 AM. I am in the labor and delivery unit propped up in a hospital bed with an IV, oxygen saturation monitor, and a fetal heart monitor on my belly. My husband is to the left of me, along with two nurses and a young male anesthesiologist elsewhere in the room. I feel tense all over and my heart begins to beat faster as I remember what happened during my last birthing experience. I ask the anesthesiologist if he had read my file in preparation for today. He says no and even shrugs when I describe my previous birthing experience. I want to scream, my jaw clenches and my stomach feels knotted, but I keep my emotions inside. I feel like everything is unraveling.”
Baby/mom attachment connection
“I’m lying on the birthing bed in the delivery room with my husband and the midwife holding my legs wide open. My heart races and I feel sweaty as the nurse tells me, “next push and she’s going to be here.” Suddenly, someone plops my baby onto me. With my eyes wide open, I look at her big purple face. It doesn’t feel like this is my baby and I feel disconnected, waiting for her to make a sound. Then, my palms are clammy as they quickly take her away and I feel shocked. She doesn’t look right, and I know that something is wrong.”
Resources for New Parents
If you or someone you care about needs mental health help, please consider calling one of these numbers on the right. If you are facing a life-threatening emergency call 911 or go to the nearest emergency department.
General Mental Health Resources
- National Suicide Prevention Hotline: 988
- Massachusetts Behavioral Health Help: 833-773-2445
- Massachusetts non-urgent help with social needs: 211
- National Crisis Text Line: Text HOME to 741741 from anywhere in the USA, anytime, about any type of crisis.
Las personas en crisis deben llamar a sus médicos, al número de emergencia local o a una de las Líneas Directas Nacionales de Emergencia que se muestran a continuación.
- Línea de Crisis Nacional- Mensaje de texto : Envia un mensaje de texto con la palabra HOME al 741741 desde cualquier lugar de los EE. UU., en cualquier momento, sobre cualquier tipo de crisis.
Postpartum and Maternal Mental Health Resources
- Postpartum Support International (PSI)
- Helpline: 1-800-944-4773. You can connect with a support coordinator near you and search their online provider directory
- NOTE: The PSI Helpline does not handle emergencies. People in crisis should call their local emergency number or the National Suicide Prevention Hotline at 1-800-273-TALK (8255).
- PSI International Resources
- PSI of Massachusetts provides toll-free and confidential information and support. Leave a message and a volunteer will get back to you within 24 hours. Call 866-472-1897 or Text “Help” to 800-944-4773
- The National Maternal Mental Health Hotline
- Helpline: 1-833-TLC-MAMA (1-833-852-6262). This free, confidential service provides access to trained counselors and resources 24 hours a day, 7 days a week in English and Spanish. They can offer support and information related to before, during, and after pregnancy.
- Massachusetts Child Psychiatry Access Program for Moms (MCPAP) promotes maternal and child health by building the capacity of providers serving pregnant and postpartum women and their children up to one year after delivery to effectively prevent, identify, and manage mental health and substance use concerns.
- Jewish Family & Children’s Services offers free Home Visiting Program for new mothers in both English and Spanish.
- Mass PPD Fund offers new parent mental health resources









Lab Presentations
See Dr. Dekel present her research into childbirth trauma and maternal PTSD.
Dr. Dekel was featured as the keynote presenter at the “Birth Trauma: Understanding Its Origins and The Urgent Need to Do More” webinar, hosted by the Policy Center for Maternal Mental Health. (December 2024)
Dr. Dekel presents “The Next Steps in Addressing Birth Trauma and Child Birth-PTSD (CB-PTSD)” at the Maternal Mental Health FORUM, hosted by the Policy Center for Maternal Mental Health. (March 2025)
Dr. Dekel presents on The Role of Gestational Diabetes in Maternal Psychiatric Pathology at the DPSG-NA 2023 Conference: 17th Biennial Meeting of the Diabetes in Pregnancy Study Group of North America, October 26-28, 2023.
Dr. Dekel presents her research on maternal wellness during COVID-19 as part of a symposium on perinatal trauma at the Marce of North America (MONA) 2021 Biennial Conference on Perinatal Mental Health.
Dr. Dekel presents her neuroimaging research on maternal PTSD at Harvard’s 2021 Mind Brain Behavior Interfaculty Initiative virtual showcase.
Podcast: The Joint Committee on the Status of Women (JCSW) Show: Mental Health After Childbirth with Assistant Professor Sharon Dekel
Through the Magnifying Glass: The Dekel Lab and the Psychiatry of Childbirth
Clinical Research
If you are pregnant and planning to give birth at MGH, and interested in participating in research, please email MothersStudy@partners.org.

Current Lab Studies
Defining Postpartum PTSD and Its Implications for Maternal Wellness and Child Development (Harvard-MGH BIRTH study)
Maternal mental illness following childbirth is associated with substantial societal costs. An estimated 240,000 American women suffer from childbirth-related post-traumatic stress disorder (CB-PTSD) each year. Some may struggle with forming an emotional attachment to their infant. Yet, CB-PTSD remains largely underdiagnosed and undertreated, and we want to change this reality through state-of-the art research. This NIH-funded study aims to define the course and predictors of CB-PTSD and its effects on the child, and establish the foundation for preventive and holistic care for both mother and child. We are studying women from the time of pregnancy and at repeated times throughout the first postpartum year. Over 500 pregnant women have been enrolled in this study so far. The study is open to enrollment for women who receive their perinatal care at MGH.
If you would like to learn more about this project, please contact our Clinical Research Coordinator Elli Dassopoulos: edassopoulos@mgh.harvard.edu
Preventing Childbirth-Related PTSD With Expressive Writing (CARES)
There are no established recommendations for interventions to prevent PTSD following childbirth. However, this form of PTSD is an ideal candidate for prevention because we know when the disorder develops, that is, after childbirth, and women are followed as part of routine care during this time period. In this first-of-its-kind study, we are testing whether a brief and early psychological intervention can prevent PTSD following a complicated, highly stressful delivery. The study is funded by the NIH and entails a randomized clinical trial, which is the state-of-the-art study design in clinical research to determine whether a treatment is effective or not. Women are asked to write about their childbirth experience or, as a control group, neutral daily events, in the first postpartum days. Our work furthers the NICHD’s mission that “women avoid harmful effects from reproductive processes and children achieve healthy and productive lives.” ClinicalTrials.gov IDNCT05662423. The study is open to enrollment for women who receive their perinatal care at MGH.
If you would like to learn more about this project, please contact our Clinical Research Coordinator Christina Pham: CPHAM4@mgh.harvard.eduOur recent publication, Preventing Posttraumatic Stress Disorder following Childbirth: A Systematic Review and Meta-analysis, published in the American Journal of Obstetrics & Gynecology (AJOG), reviews options for interventions to prevent or treat childbirth-related PTSD, and offers recommendations for the most effective strategies currently known.
Global Mental Health Initiative: Harvard-Israel Birth Study
Although large-scale man-made trauma remains a global threat, our knowledge about the impact of terrorism and war on birth outcomes is scarce. This is in part because it is difficult to develop a study during times of crisis. We are collaborating with teams in Israel to study the impact of the October 7th massacre and the Israel-Hamas War on pregnant and postpartum women residing in Israel. Our goal is to collect critical information on women’s mental health and understand how heightened levels of stress may affect birth outcomes. We have enrolled over 1200 women so far, and we are conducting our second phase of data collection.
Global Mental Health Initiative: Nigerian Obstetric Wellness (NOW) Project
The study of maternal mental health in developing countries is lacking. Unfortunately, rates of maternal death remain high in certain regions of the world, and accordingly, so do severe complications in childbirth that likely result in developing PTSD. Nigeria is among the leading countries in which the state of maternal mental health is poor: 1,047 out of 100,000 women die from complications related to pregnancy and childbirth, with an associated psychological toll. We have collaborated with the Obstetrics and Gynaecology Department of the University College Hospital in Ibadan, Nigeria (Site PI: Prof. Adesina Oladokun) to perform the first-ever study on traumatic childbirth and PTSD. We are investigating the prevalence of maternal PTSD and its risk factors by studying patients in this hospital. We are interested in revealing how social determinants of health, as well as the actual practice of perinatal care, impacts women’s well-being.
Preventing Postpartum Depression with Oxytocin
Our NIH-funded clinical trial introduces a novel therapeutic approach with the use of oxytocin administered to mothers at risk immediately following childbirth. We are testing whether oxytocin, an anxiolytic and pro-social hormone, can reduce postpartum depression and anxiety and boost mother-infant bonding as well as breastfeeding to the ultimate benefit of the child’s health. Boosting mother-infant bonding at a critical stage for infant development can modify the long-term health trajectory of the child. This study is done in collaboration with an interdisciplinary team of Mass General researchers and the Mass General Obstetrics Program. This study is currently in the data analysis phase. Clinical Trial
The Maternal Brain: Examining Neural Alterations Following Traumatic Childbirth
As many as a third of women experience a traumatic childbirth, and a significant portion can go on to develop PTSD (CB-PTSD). Nevertheless, research on the underlying biological mechanisms of this maternal condition that can establish disease biomarkers is completely lacking. Neuroimaging is currently the only technique that provides direct, non-invasive access to the living human brain. This NIH-funded study is the first of its kind to examine potential changes in the maternal brain associated with traumatic childbirth and the development of CB-PTSD. We use magnetic resonance imaging (MRI) tasks to reveal the core neural abnormalities of childbirth-related PTSD and how these abnormalities can mediate problems in early mother-infant attachment and impair healthy child development. Elucidating the neural correlates of postpartum PTSD and yielding clinically relevant biomarkers could translate into the development of new therapies and improve clinical diagnosis. This study is currently in the stage of data analysis; we look forward to sharing our findings soon.
In our paper published in the American Journal of Obstetrics & Gynecology (AJOG), A Diagnostic Questionnaire for Childbirth Related Posttraumatic Stress Disorder: A Validation Study, we show that the Posttraumatic Stress Disorder Checklist for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (PCL-5) questionnaire can be used as an accurate screening tool for CB-PTSD.
Childbirth-induced Postpartum Psychological Outcomes
Identifying women at risk for postpartum mental health disorders is crucial for implementing preventive treatment tailored to different symptoms. In this NIH-funded large-scale prospective, longitudinal study, we are examining women’s mental health trajectories from pregnancy through childbirth into the early postpartum period. We study the experience of childbirth and subsequent heterogeneous psychological responses to better capture the dynamic nature of postpartum coping over time. We assess negative as well as positive mental health outcomes induced by the childbirth experience and the factors predicting these responses. This study enrolled women who were pregnant at MGH; over 1,500 subjects have been enrolled, and we are in the phase of data analysis.
Traumatic Childbirth: A Physiological Approach to Study Maternal Posttraumatic Stress Disorder
International Study of Childbirth Characteristics and Subsequent PTSD
We completed a study of over 800 postpartum women from around the globe, targeting posttraumatic stress symptoms following childbirth. We have found that as many as 12% of women are expected to experience PTSD symptoms at a clinical level after giving birth to a healthy baby at term. Women who have an unscheduled Cesarean are three times more likely to suffer from PTSD.
Overall, our findings show that objective stressors in birth, such as mode of delivery and obstetrical complications, as well as the woman’s subjective traumatic experience of childbirth, including peritraumatic dissociation, predict the development of subsequent PTSD. Socioeconomic disadvantage also increases vulnerability, as does a prior history of sexual assault. Furthermore, having symptoms of PTSD can interfere with the mother’s ability to bond with her baby. We also found differences in cortisol response to trauma in women with and without comorbid PTSD and depression. Using written narratives about the childbirth experience, we found that the narratives of women with CB-PTSD are characterized by less affective and more cognitive descriptions, and that trauma memories of women with CB-PTSD are similar to those reported for other forms of PTSD. However, we also found that the childbirth experience may lead to post-traumatic growth.
Impact of Coronavirus on Mothers' Birth Experience and Wellbeing
The outbreak of the COVID-19 pandemic turned the lives of millions of people upside down all over the globe and affected our wellbeing. Our mothers wellness coronavirus project was an international study open to all women in the U.S. and other countries; over 4,000 women were enrolled. This NIH-funded study yielded extensive findings that have been published in six journal articles.
- We found that mothers in COVID-19-exposed communities endorsed more clinically acute stress response to childbirth than matched controls. Acute stress mediated the relationship between study group and postpartum outcomes. (PMID33412491)
- Nearly 50% of COVID-19-positive women endorsed acute traumatic stress symptoms at a clinical level in response to childbirth. This group was more than twice as likely to endorse acute stress and to have no visitors during maternity hospitalization than COVID negative women. The COVID-19-positive group reported higher levels of pain in delivery, lower newborn weights, and more infant admission to neonatal intensive care units (PMID34188137).
- >60% of participants reported childbirth-related post-traumatic growth (PTG), with greater appreciation of life endorsed most frequently. In deliveries during the pandemic, childbirth-related acute stress was linked with elevated PTG; in turn, PTG was associated with lower posttraumatic stress symptoms and better mother-infant bonding. (PMID35772629)
- We used a machine learning-based natural language processing model to represent childbirth narratives as vectors that served as inputs for a neural network machine learning model to identify participants with childbirth-related posttraumatic stress disorder (CB-PTSD). (PMID36509356)
- We used numerical vector representations of childbirth narratives and compared ChatGPT vs. other machine learning (ML)-based large language models to assess for CB-PTSD, and we developed a model that performs very well (F1 score: 0.81). (PMID37886525)
- We demonstrated the feasibility of using the Peritraumatic Distress Inventory (PDI) to assess for acute distress to classify women likely to endorse CB-PTSD. The data used in this study is also related to our International Survey. (PMID38070747)
Research Team

Sharon Dekel, PhD | Principal Investigator
Dr. Sharon Dekel is an Associate Professor of Psychology at Harvard Medical School (HMS) and the Director of the Postpartum Traumatic Stress Disorders Research Program at Massachusetts General Hospital (MGH) and the Dekel Lab at HMS and MGH. She earned a PhD in Clinical Psychology from Columbia University and completed her clinical internship training at Columbia Medical Center followed by a research postdoctoral fellowship in a leading international Trauma lab. Dr. Dekel is also a licensed clinical psychologist.
Dr. Dekel has been studying biological and psychological factors associated with ways of coping with stressful events. Her work on the positive outlook of traumatic stress is considered pioneering in the field. Rather than viewing trauma outcomes as exclusively negative, her studies have increased our understanding of the human capacity to thrive in the wake of trauma.
Since joining Massachusetts General Hospital in 2013, Dr. Dekel has expanded her research with the investigation of childbirth as a potentially traumatic event (see Dr. Dekel's publication record). This represents a new frontier in trauma studies. She developed a multidisciplinary research model involving both the Mass General Psychiatric and OB/GYN Departments that has allowed her to study over 8,000 postpartum women. Dr. Dekel is defining the overlooked condition of childbirth-related post-traumatic stress disorder (CB-PTSD) and working to better understand the transmission of the disorder’s effects to the offspring. By studying childbirth as a model of traumatic stress, she hopes to translate the knowledge gained to improve clinical care of trauma-exposed individuals.
Dr. Dekel has also been honored for her exceptional mentorship: She was awarded the 2025 Harvard Medical School's Joint Committee on the Status of Women (JCSW) Shirley Driscoll Dean’s Leadership Award for the Enhancement of Women’s Careers, and she was named the recipient of the 2025 International Society for Traumatic Stress Studies (ISTSS) Distinguished Mentorship Award.
Dr. Dekel is a two-time recipient of the Brain and Behavior Research Foundation’s Young Investigator Award, the MGH’s Executive Committee On Research ISF funding, and the Harvard Mind Brain Behavior Faculty Award. She also received Mass General’s Claflin Distinguished Scholar Award for Women in Science, and is a recent recipient of Postpartum Support International Susan A. Hickman Memorial Research Award for excellence in scientific work on postpartum mental health. She has been continually supported by the National Institutes of Health.
Dr. Dekel is on the Editorial Boards of PLOS ONE, Archive of Women’s Mental Health, the Annals of Depression and Anxiety, Frontiers in Psychiatry, Frontiers in Psychology, where she edited a special volume on childbirth-related PTSD, and the journal Psychological Trauma: Theory, Research, Practice, and Policy, the American Psychological Association’s leading traumatic stress journal. Dr. Dekel serves on the Board of the International Marcé Society, the largest organization supporting perinatal mental health. She is also the founding Chair of the Postpartum Trauma Special Interest Group of the International Society of Traumatic Stress Studies, which is the largest professional organization in the field.
Postdoctoral Research Fellows

Hadas Allouche-Kam, MD
Hadas Allouche-Kam, MD, is an Israeli specialist in obstetrics and gynecology. She completed her medical training and residency at the Hebrew University and the Hadassah Medical Center in Israel. During her experience in the delivery room, she witnessed how labor and delivery can cause physical and mental stress that may have a long-term impact. She consequently contributed to establishing the Healing Birth Clinic in Israel, treating women with previous birth trauma or other relevant histories to minimize re-traumatization in upcoming birth. In her work in the Dekel Laboratory, she investigates which obstetric factors have an influence on traumatic experiences related to birth, and how such trauma can be prevented. In addition, she investigates the impact of the October 7 massacre and the Hamas-Israel War on the mental and physical well-being of Israeli women during pregnancy and in the postpartum period.

Kelimer Lebrón-Sagardia, PhD
Dr. Kelimer Lebrón-Sagardia is a Latina neuroscientist focused on research related to women's mental health. From her early work at Ponce Health Science University, Puerto Rico, to her postdoctoral tenure at Massachusetts General Hospital and Harvard Medical School, she has explored fear extinction in anxiety disorders. Her foundational research links gonadal hormonal fluctuations to an elevated risk of anxiety disorders in women. As a Research Fellow in Dr. Dekel's lab, supported by an NIH Re-Entry Supplement, Dr. Lebrón-Sagardia focuses on maternal mental health, studying racial discrimination's impact on Black and Hispanic postpartum women. Committed to addressing maternal health disparities, she strives to innovate healthcare strategies for her community.

Kathleen Jagodnik, PhD
Kathleen is a researcher with a passion for exploration and innovation, focusing on maternal mental health. She earned her MS and PhD degrees in Biomedical Engineering from Case Western Reserve University in Cleveland, Ohio. Her work in the Dekel Lab focuses on using Machine Learning to identify risk factors of childbirth-associated PTSD (CB-PTSD) and developing computational models to estimate women’s risk for CB-PTSD. She authored several publications with the Dekel Lab (PMID 37162947, PMID 38122842, PMID 37981091 , PMID 38149098), including two studies involving the use of Machine Learning to analyze childbirth narratives to assess for CB-PTSD (PMID 36093354, PMID 37886525) and a book chapter on CB-PTSD. In her free time, she enjoys spending time with friends, reading, composing electronic music, conducting completist music reviews, and pursuing various creative projects.
PhD Graduate Student

Gabriella Hamlett, MA
Gabriella completed her MA degree at Teachers College, Columbia University in 2020 and her B.S. at UC Davis in 2017. She is a Clinical Psychology PhD student at Harvard University. She is interested in emotion regulatory processes underlying the onset and maintenance of PTSD, anxiety, and OCD, particularly in peripartum women. She is conducting her PhD project in the Lab where she is using network analysis to study the dynamic relationships among trauma symptoms, emotion regulation, and external factors across the perinatal period.
Clinical Research Coordinators

Onyekachi Agwu, BA
Onyeka earned her BA degree in Neurobiology from Harvard University. As a CRC in the Dekel Lab, she leads the coordination of the BIRTH Study, assists with the Expressive Writing Study, and conducts physiological assessments. She is a coauthor on the Dekel Lab’s preliminary review of peritraumatic dissociation during childbirth in Nigeria (PMID: 40391551). In her free time, Onyeka enjoys dancing and cooking. In the future, she hopes to attend medical school and specialize in Neurology.

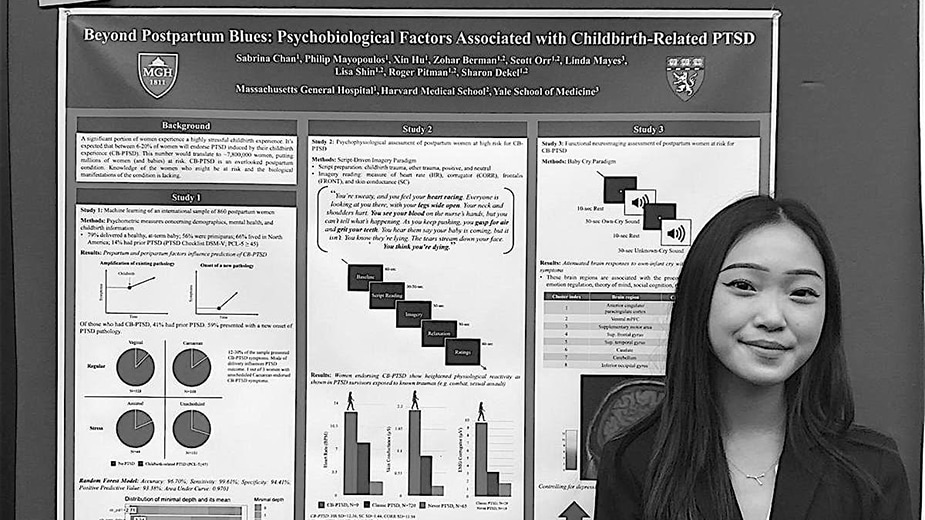
Sabrina Chan, BS
Sabrina earned her BS degree in Behavioral Neuroscience from Northeastern University and conducted her honors thesis in the Lab on the effect of intranasal oxytocin on postpartum depression and maternal infant bonding. Over the course of her time in the Lab, she has authored 12 publications (PMID 36093354, PMID 37886525, PMID 37162947, PMID 35598158, PMID 35772629, PMID 34188137, PMID 33412491, PMID 33276245, PMID 32705348), of which two are first author (PMID 32480118, PMID 35640702) and 1 is co-first author (PMID 35772629). Sabrina has presented her work in two poster presentations at the ISTSS conference (2019, 2020). She will matriculate to a Medical Scientist Training Program (MSTP) beginning in summer 2024 to combine her passion for clinical and translational research with the ability to treat mental and physical health holistically.

Elli Dassopoulos, BA
Elli graduated from the Dual BA Program between Columbia University and Sciences Po, with degrees in Psychology, Comparative Literature, and Political Humanities. In the Dekel Lab, she coordinates the BIRTH Study on postpartum PTSD, in which she conducts assessments with mothers and children. Outside of her work at the Dekel Lab, Elli loves to learn languages, draw, and read psychoanalytic theory. She hopes to pursue a PhD in clinical psychology and eventually work as a psychoanalyst and professor.

Ananya Iyengar, BS
Ananya graduated from Northeastern University, where she studied Biology, Psychology, and Behavioral Neuroscience. She joined the Lab in the spring of 2021, as part of Northeastern’s co-op program, and has primarily worked on assessing mother-infant interactions and postpartum PTSD as part of the Maternal Brain Study. She is first author on the Dekel Lab publication PMID 35598158. She plans to attend medical school in the future. Outside of school and research, Ananya enjoys traveling and plant-based cooking.

Mary Lee, BA
Mary graduated from Northeastern University, where she studied Health Science with a minor in Biology. In the Dekel Lab she aids in the coordination of the BIRTH Study. In the future, Mary hopes to attend medical school to become an OB/GYN or primary care doctor. She enjoys spending time with friends and family, playing guitar, reading, and painting.

Christina Pham, BA
Christina graduated from Harvard College, where she studied English Literature with a minor in Mind, Brain, and Behavior. In the Dekel Lab, she leads coordination for the Expressive Writing study, assists with the BIRTH study, and conducts child developmental assessments. She is a coauthor on the Dekel Lab’s systematic review and meta-analysis of interventions to prevent and treat childbirth-related PTSD (CB-PTSD) (PMID 38122842). She hopes to attend medical school in the future. In her free time, Christina enjoys writing and traveling.
Research Interns

Sarah Adam
Sarah is a fourth-year undergraduate student at Harvard College studying Psychology on the Pre-Medical track with a secondary in Global Health and Health Policy (GHHP). As a Research Intern in the Dekel Lab, she primarily assists with the BIRTH study, which focuses on postpartum PTSD. For her future aspirations, Sarah hopes to one day attend medical school and become a psychiatrist, particularly to help those in under-resourced communities get access to mental healthcare. Outside of academics and research, she loves to binge watch her favorite shows (One Piece and Love is Blind), listen to and make music, and try out new food places all around Boston.

Eunice Chon
Eunice is a fourth-year undergraduate at Harvard College studying History of Science and Philosophy, with an additional interest in Global Health and Health Policy. Currently, she contributes to the BIRTH Study and Harvard Israel Study at the Dekel Lab. In the future, Eunice hopes to attend medical school to become an OB/GYN and graduate school to become a historian of medicine and medical ethicist. She is passionate about disability advocacy and law, including mental health justice and activism.
Fajr Khan
Fajr is a fourth-year undergraduate at Harvard College studying Neuroscience and Philosophy. As a research intern at the Dekel Lab, Fajr primarily contributes to the BIRTH study. She is from The Netherlands and Pakistan, and is passionate about improving women’s mental health in resource-limited settings. Fajr plans to pursue a PhD in Clinical Psychology or attend medical school. Outside of the lab, Fajr enjoys reading, going to spin classes, and trying out new cafés.
Sophia Meadors
Sophia is a fourth-year undergraduate student at Northeastern University studying Behavioral Neuroscience. At the Dekel Lab, Sophia contributes to the BIRTH Study as a research intern. In the future, she hopes to attend medical school to become a surgeon. In her free time, she loves to read, go on walks, cook for her family and friends, and play with her four German shepherds.

Chinasa Ohajekwe
Chinasa is a fourth-year undergraduate student at Harvard College studying Neuroscience in the Mind, Brain, and Behavior Track with a secondary in Economics and a citation in Spanish. As a research intern in the Dekel Lab, she primarily assists the BIRTH study involving postpartum PTSD. She hopes to attend medical school to work in neurology or OB/GYN and to serve underprivileged areas in New York City. In her free time, she enjoys taking photos of friends, trying new foods, and watching movies.

Jiajia Zhang
Jiajia is a third-year undergraduate student at Harvard University. She is studying Human Evolutionary Biology and languages (ASL and Spanish). She is currently a research intern with the Dekel Lab and is assisting in the BIRTH study and Expressive Writing Study. After college, Jiajia plans to attend medical school, with a special interest in becoming a surgeon or primary care doctor. She loves sports, especially endurance races like Spartan 10k and Olympic-distance Triathlons.
Computational Team
Isha Aurora
Isha Arora earned her MS in Data Science from Northeastern University. As a Data Analyst in the Dekel Lab, she supports a range of research studies, with a primary focus on the BIRTH Study on postpartum PTSD. With a strong foundation in data science and a deep interest in health equity, Isha applies advanced statistical methods and data visualization to uncover insights from complex datasets—helping to illuminate the psychological impacts of childbirth on women. She also provides analytic support across multiple ongoing projects in the lab, working closely with clinicians and researchers to advance understanding and improve outcomes in maternal mental health.
Collaborators
List of collaborators
- Alon Bartal, PhD, Bar-Ilan University
- Sara Bates, MD, Massachusetts General Hospital, Harvard Medical School
- George Bonanno, PhD, Columbia University
- Tsachi Ein Dor, PhD, Reichman University, Israel
- Ruth Feldman, PhD, Reichman University, Israel
- Lauren Hanley, MD, Massachusetts General Hospital, Harvard Medical School
- Anjali Kaimal, MD, University of South Florida
- Elizabeth Lawson, MD, Massachusetts General Hospital, Harvard Medical School
- Linda Mayes, MD, Yale University
- Scott Orr, PhD, Massachusetts General Hospital, Harvard Medical School
- Roger Pitman, MD, Massachusetts General Hospital, Harvard Medical School
- Jeffery Rosen, PhD, University of Delaware
- Lisa Shin, PhD, Tufts University
- Zahava Solomon, PhD, Tel Aviv University, Israel
- Ahmed Tawakol, MD, Massachusetts General Hospital, Harvard Medical School
- Peter Tsvetkov, PhD, Broad Institute
Research Positions

We have ongoing research opportunities in our lab. To learn about postdoctoral and research fellowship positions, please contact Dr. Sharon Dekel at sdekel@mgh.harvard.edu
Research Volunteers: We are seeking student volunteers to assist with the operation of ongoing clinical research studies in our lab. Primarily responsibilities will involve screening candidates and recruiting subjects, data entry, and assisting with conducting the biological and psychological assessments of subjects as needed. Ideal candidates will be highly motivated with the strong interpersonal skills necessary to interact with patients and succeed in a dynamic work environment. If you are interested, please send your cover letter and resume to our clinical research coordinator, Ms. Christina Pham at cpham4@mgh.harvard.edu.
News, Achievements, and Publications
Lab Achievements and News Mentions
- Dr. Dekel was awarded an R01 grant from the NIH National Institute of Child Health and Human Development (NICHD) titled “Establishing a Screening Tool for Early Detection of PTSD Following Complicated Childbirth” to develop an Artificial Intelligence (AI) model for the early detection of PTSD following childbirth trauma. (September 2025)
- Dr. Dekel is the recipient of an 2025 MGH Executive Committee on Research (ECOR) ISF Research Award supporting her work on detecting childbirth-related PTSD (CB-PTSD) using AI-based computational models. (July 2025)
View all lab achievements and news mentions (PDF)
Selected Publications (Most recent first)
Peritraumatic dissociation during childbirth in Nigeria: A preliminary study Akinwunmi B, Adeyanju AS, Arora IH, Quagliarini B, Agwu O, Oladokun A, Dekel S. Int J Gynaecol Obstet. 2025 Oct;171(1):460-463. doi: 10.1002/ijgo.70214. Epub 2025 May 20. PMID: 40391551; PMCID: PMC12456323.
Targeted Research and Treatment Implications in Women With Depression. Gaine ME, Jagodnik KM, Baweja R, Bobo WV, McGlade EC, Weiss SJ, Beal ML, Dekel S, Ozerdem A. Focus: The Journal of Lifelong Learning in Psychiatry. 23(2), pp.141-155. April 15, 2025. PubMed PMID: 40235608, DOI: 10.1176/appi.focus.20240052.
Partner Military Deployment and War Conditions Increase Perinatal Depression and Decrease Postpartum Mother-Infant Bonding. Allouche-Kam H, Chan SJ, Arora IH, Pham CT, Reuveni I, Sheiner E, Dekel S. medRxiv, pp.2025-01. March 17, 2025.
Brain Health Begins Before Birth (B4): A “Learning” Pregnancy and Birth Cohort Study. Pride RL, Villarreal J, Restrepo D, Grunberg VA, Bazan M, Subedi D, Fitzgerald A, Shauh K, Wollman E, Perdomo S, Bazer OM. medRxiv, pp.2025-03. March 13, 2025.
Network Analysis of PTSD Symptoms Following Childbirth and Comorbid Conditions Among Women with Sexual Trauma History. Hamlett GE, McGhie SF, Dishy G, Chan SJ, McNally RJ, Dekel S. Arch Womens Ment Health. 2025 Mar 12; DOI: 10.1007/s00737-025-01570-5. [Epub ahead of print] PubMed PMID: 40072580; NIHMSID:NIHMS2068334
Understanding the Link Between Cesarean Delivery and Childbirth-related Posttraumatic Stress Disorder. Dekel S, Hughes F. Am J Obstet Gynecol. 2025 Jan 30; DOI: 10.1016/j.ajog.2025.01.034. [Epub ahead of print] PubMed PMID: 39892839.
The Association of Delivery During a War with the Risk for Postpartum Depression, Anxiety and Impaired Maternal-Infant Bonding, A Prospective Cohort Study. Klapper-Goldstein H, Pariente G, Wainstock T, Dekel S, Binyamin Y, Lanxner Battat T, Wissotzky Broder O, Kosef T, Sheiner E. 2024. Archives of Gynecology and Obstetrics. October 5, 2024. pp. 1-9. PMID: 39367974. DOI: 10.1007/s00404-024-07715-8
Childbirth-Related Post-Traumatic Stress Disorder. Dekel S, Chan SJ, Jagodnik KM. 2024. The Routledge International Handbook of Perinatal Mental Health Disorders, 1st Edition. pp. 330-357. Routledge.
Establishing the Validity of a Diagnostic Questionnaire for Childbirth-related Posttraumatic Stress Disorder: A Reply. Dekel S, Orr SP. 2024. American Journal of Obstetrics & Gynecology, May, 230(5), p. e102. PMID: 38158073. DOI: 10.1016/j.ajog.2023.12.026
AI and Narrative Embeddings Detect PTSD following Childbirth via Birth Stories. Bartal A, Jagodnik KM, Chan SJ, Dekel S. Scientific Reports. 2024. 14(1): 8336. PMID: 38605073 DOI: 10.1038/s41598-024-54242-2A Call for a Formal Diagnosis for Childbirth-related PTSD. Dekel S. Nature Mental Health. 2024. 2:259-260. https://doi.org/10.1038/s44220-024-00213-5
Screening for Post-Traumatic Stress Disorder Following Childbirth Using the Peritraumatic Distress Inventory. Jagodnik KM, Ein-Dor T, Chan SJ, Titelman Ashkenazy A, Bartal A, Dekel S. Journal of Affective Disorders. 2024. 1 March 2024, 348:17-25. PMID: 37162947 DOI: https://doi.org/10.1016/j.jad.2023.12.010
Anxiety Disorders and Post-traumatic Stress Disorder. Baker AW, Dekel S, Jagodnik KM, Pace-Schott EF, Post LM, Orr SP. Chapter 31 in Massachusetts General Hospital Comprehensive Clinical Psychiatry, Eds. Stern TA, Wilens TE, and Fava M. 2024.
Preventing Post-Traumatic Stress Disorder Following Childbirth: A Systematic Review and Meta-Analysis. Dekel S, Papadakis J, Quagliarini B, Pham CT, Pacheco-Barrios K, Hughes F, Jagodnik KM, Nandru R. American Journal of Obstetrics & Gynecology (AJOG). 2024. Volume 230, Issue 6, June, Pages 610-641.e14. PMID: 38122842 https://doi.org/10.1016/j.ajog.2023.12.013
A Diagnostic Questionnaire for Childbirth Related Posttraumatic Stress Disorder: A Validation Study. Arora IH, Woscoboinik GG, Mokhtar S, Quagliarini B, Bartal A, Jagodnik KM, Barry RL, Edlow AG, Orr SP, Dekel S. American Journal of Obstetrics & Gynecology (AJOG). 2023. In Press; Available online 21 November 2023. PMID: 37981091 DOI: https://doi.org/10.1016/j.ajog.2023.11.1229
The Role of the Hypothalamic-Pituitary-Adrenal Axis in Depression across the Female Reproductive Lifecycle: Current Knowledge and Future Directions. Hantsoo L, Jagodnik KM, Novick AM, Baweja R, Lanza di Scalea T, Ozerdem A, McGlade EC, Simeonova DI, Dekel S, Kornfield SL, Nazareth M, Weiss SJ. Frontiers in Endocrinology. 2023. Volume 14. PMID: 38149098 DOI: https://doi.org/10.3389/fendo.2023.1295261
Increased traumatic childbirth and postpartum depression and lack of exclusive breastfeeding in Black and Latinx individuals. Iyengar AS, Ein-Dor T, Zhang EX, Chan SJ, Kaimal AJ, Dekel S. Int J Gynaecol Obstet. 2022 May 22. PMID: 35598158. DOI: 10.1002/ijgo.14280
Peripartum effects of synthetic oxytocin: The good, the bad, and the unknown. Rashidi M, Maier E, Dekel S, Sütterlin M, Wolf RC, Ditzen B, Grinevich V, Herpertz SC. Neuroscience and Biobehavioral Reviews 141. 2022,104859. PMID:36087759. DOI: 10.1016/j.neubiorev.2022.104859
Identifying Women with Post-Delivery Posttraumatic Stress Disorder using Natural Language Processing of Personal Childbirth Narratives. Bartal A, Jagodnik KM, Chan MSJ, Babu MMS, Dekel S. Am J Obstet Gynecol MFM. 2022 Dec 9; 100834. doi: 10.1016/j.ajogmf.2022.100834. PubMed PMID: 36509356; NIHMSID:NIHMS1856600.
Traumatic childbirth during COVID-19 triggers maternal psychological growth and in turn better mother-infant bonding. Babu MS, Chan SJ, Ein-Dor T, Dekel S. J Affect Disord. 2022 Jun 27; 313:163-166. PMID: 35772629. PMCID: PMC7889625 DOI: 10.1016/j.jad.2022.06.076
Validation of Childbirth-Related Posttraumatic Stress Disorder Using Psychophysiological Assessment. Chan SJ, Thiel F, Kaimal AJ, Pitman RK, Orr SP, Dekel S. Am J Obstet Gynecol. 2022 May 28. PMID: 35640702. DOI: 10.1016/j.ajog.2022.05.051
Increased traumatic childbirth and postpartum depression and lack of exclusive breastfeeding in Black and Latinx individuals. Iyengar AS, Ein-Dor T, Zhang EX, Chan SJ, Kaimal AJ, Dekel S. Int J Gynaecol Obstet. 2022 May 22. PMID: 35598158.
COVID‑19 positivity associated with traumatic stress response to childbirth and no visitors and infant separation in the hospital. Mayopoulos GA, Ein-Dor T, Li KG, Chan SJ, Dekel S. Scientific Reports. 2021, 11:1353; DOI: 10.1038/s41598-021-92985-4 PMID: 34188137
Association of sexual assault history with traumatic childbirth and subsequent PTSD. Berman Z, Thiel F, Kaimal AJ, Dekel S. Archives of Women’s Mental Health. 2021. DOI: 10.1007/s00737-021-01129-0. PMID: 33847820
COVID-19 is associated with traumatic childbirth and subsequent mother-infant bonding problems. Mayopoulos GA, Ein-Dor T, Dishy GA, Nandru R, Chan SJ, Hanley LE, Kaimal AJ, Dekel S. Journal of Affective Disorders. 2021; DOI: 10.1016/j.jad.2020.12.101 PMID: 33412491
Traumatic memories of childbirth relate to maternal postpartum posttraumatic stress disorder. Thiel F, Berman Z, Dishy GA, Chan SJ, Seth H, Tokala M, Pitman RK, Dekel S. Journal of Anxiety Disorders. 2021;77: 102342. DOI: 10.1016/j.janxdis.2020.102342. PMID: 33276245
Maternal psychological growth following childbirth. Berman Z, Thiel F, Dishy GA, Chan SJ, Dekel S. Archives of Women’s Mental Health. 2020. DOI: 10.1007/s00737-020-01053-9. PMID: 33276245
Risk factors for developing posttraumatic stress disorder following childbirth. Chan SJ, Ein-Dor T, Mayopoulos P, Mesa M, Sunda R, McCarthy B, Kaimal A, Dekel S. Psychiatry Research. May 2020;290: 113090. PMID: 32480118 DOI: 10.1016/j.psychres.2020.113090
Beyond postpartum depression: Posttraumatic stress-depressive response following childbirth. Dekel S, Ein-Dor T, Dishy G, Mayopoulos P. Archives of Women’s Mental Health. 2020;23: 557-564. DOI:10.1007/s00737-019-01006-x. PMID: 31650283
Peritraumatic dissociation in childbirth-evoked posttraumatic stress and postpartum mental health. Thiel F, Dekel S. Archives of Women’s Mental Health. 2019; 23: 189-197. PMID: 31115689. DOI: 10.1007/s00737-019-00978-0
Delivery mode is associated with maternal mental health following childbirth. Dekel S, Ein-Dor T, Berman Z, Barsoumian I, Agarwal S, Pitman RK. Archives of Women’s Mental Health. 2019; 22: 817–824. PMID: 31041603. DOI: 10.1007/s00737-019-00968-2
Dynamic course of peripartum depression across pregnancy and childbirth. Dekel S, Ein-Dor T, Ruohomäki, A, Lampi J, Voutilainen S, Tuomainen TP, Heinonen S, Kumpulainen K, Pekkanen J, Keski-Nisula L, Pasanen M, Lehto SM. Journal of Psychiatric Research. 2019; 113:72-78. PMID: 30921631.
Is childbirth-induced PTSD associated with low maternal attachment? Dekel S, Thiel F, Dishy G, Ashenfarb A. Archives of Women’s Mental Health. 2019; 22:119-122. PMID: 29786116. DOI: 10.1007/s00737-018-0853-y
Examining symptom clusters of childbirth-related posttraumatic stress disorder. Thiel F, Ein-Dor T, Dishy G, King A, Dekel S. The Primary Care Companion for CNS Disorders. 2018; 20(5). PMID: 30277674.
Differences in cortisol response to trauma activation in individuals with and without comorbid PTSD and depression. Dekel S, Ein-Dor T, Rosen JB, Bonanno GA. Frontiers in Psychology. 2017; 8:797. PMID: 28572779.
Childbirth induced posttraumatic stress syndrome: A systematic review of prevalence and risk factors. Dekel S, Stuebe C, Dishy G. Frontiers in Psychology. 2017; 8:560. PMID: 28443054. DOI: 10.1007/s00737-018-0853-y
Peripartum depression, traditional culture, and Israeli society. Dekel S, Stanger V, Georgakopoulos ER, Stuebe CM, Dishy GA. Journal of Clinical Psychology. 2016; 72(8):784-94. PMID: 27487164.
PTSD symptoms lead to modification in the memory of the trauma: a prospective study of former prisoners of war. Dekel S, Solomon Z, Ein-Dor T. The Journal of Clinical Psychiatry. 2016; 77(3):e290-6. PMID: 26796992.
Posttraumatic stress disorder and depressive symptoms: joined or independent sequelae of trauma? Dekel S, Solomon Z, Horesh D, Ein-Dor T. Journal of Psychiatric Research. 2014; 54:64-9. PMID: 24703578.
Cortisol and PTSD symptoms among male and female high-exposure 9/11 survivors. Dekel S, Ein-Dor T, Gordon KM, Rosen JB, Bonanno GA. Journal of Traumatic Stress. 2013; 26(5):621-5. PMID: 24030869.
Changes in trauma memory and patterns of posttraumatic stress. Dekel S, Bonanno G. Psychological Trauma: Theory, Research, Practice and Policy. 2013; 5(1):26-34.
Secondary salutogenic effects in veterans whose parents were Holocaust survivors? Dekel S, Solomon Z, Rozenstreich E. Journal of Psychiatric Research. 2013; 47(2):266-71. PMID: 23168139.
Self-enhancement among high-exposure survivors of the September 11th terrorist attack: resilience or social maladjustment? Bonanno GA, Rennicke C, Dekel S. Journal of Personality and Social Psychology. 2005; 88(6):984-98. PMID:15982117.
View all publications from the Dekel Lab
Podcasts
- Previa Alliance Podcast: Birth Trauma Awareness Week with Dr. Sharon Dekel
- Understanding Birth Trauma: Insights with Dr. Sharon Dekel Show: Planet Motherhood with Dr. Oscar
- The Joint Committee on the Status of Women (JCSW) Show: Mental Health After Childbirth with Assistant Professor [Now Associate Professor] Sharon Dekel
Over 60 specialty psychiatry clinical and research programs
We provide care for patients of any age throughout the lifespan.
Pioneering Psychiatry Research
The integration of patient care and clinical research has been a hallmark of the Department of Psychiatry for more than 30 years. Today, the department has the largest clinical research program in the hospital, with studies at the forefront of neuroscience, molecular biology and genetics.
