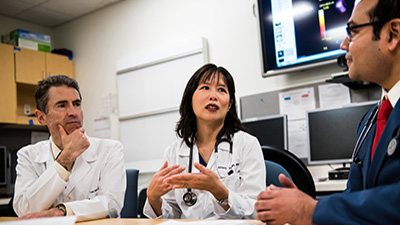
Mass General Cancer Center Receives Largest Donation in its History to Fuel Cancer Research
The newly named Krantz Family Center for Cancer Research will empower Mass General Cancer Center researchers to tackle the major unsolved challenges in oncology.
Read more