McCance Center for Brain Health


Brain Health and Alzheimer’s Disease: State of the Science
McCance Center Director Dr. Rudolph Tanzi's lecture on the state of the science in brain health and Alzheimer's disease.
McCance Center Clinical Trials Program
Drs. Rudy Tanzi and Gene Bowman discuss upcoming clinical trials at the McCance Center.
Lifestyle Changes May Slow AD Progression
Clinical trial demonstrates that lifestyle changes may slow the progression of AD, improve cognition and function.
Dr. Rudy Tanzi Talks about SHIELD in a Podcast (Part 1)
Dr. Tanzi spoke with BrainStorm podcast host Meryl Comer about the latest brain health research (part 1 of 2).
Dr. Rudy Tanzi - Alzheimer's Updates and Developments; What's New for 2025?
Dr. Tanzi joined BrainStorm host Meryl Comer to discuss Alzheimer's updates and developments.
Use the SHIELD Plan to Remember to Take Care of Your Brain
Dr. Tanzi’s SHIELD plan can improve your brain health and reduce the risk for future brain disease.
Panel Discussion on Precision Medicine Approach to Alzheimer's Disease
Speakers, including Dr. Tanzi, address the key question "How are the latest approaches and cutting-edge modalities giving health professionals an edge against Alzheimer’s?"
Foods That Improve Memory
Dr. Rudy Tanzi recommends foods that prevent dementia and other cognitive decline.
How Exercise Protects the Brain
Researchers at Massachusetts General Hospital believe they've discovered the hormonal link that allows exercise to reduce Alzheimer’s disease risk.
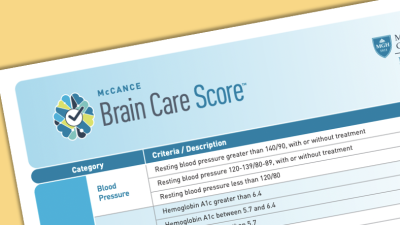
Brain Health Begins with Brain Care
McCance faculty position brain care in the spotlight, in this November 2022 Lancet Op Ed.
Neuroinflammation and Alzheimer’s Disease Risk
Alzheimer's disease (AD): Tackling neuroinflammation for early intervention and enhanced treatments
Music, Memory, and Alzheimer’s Disease
Despite dementia, 95-year-old piano player remembers every note.
News & Announcements from the McCance Center
Support The McCance Center
Help us leverage our unique positioning in the brain health community to make the scientific discoveries needed to allow us to accurately measure brain health and integrate preventive strategies into primary care.